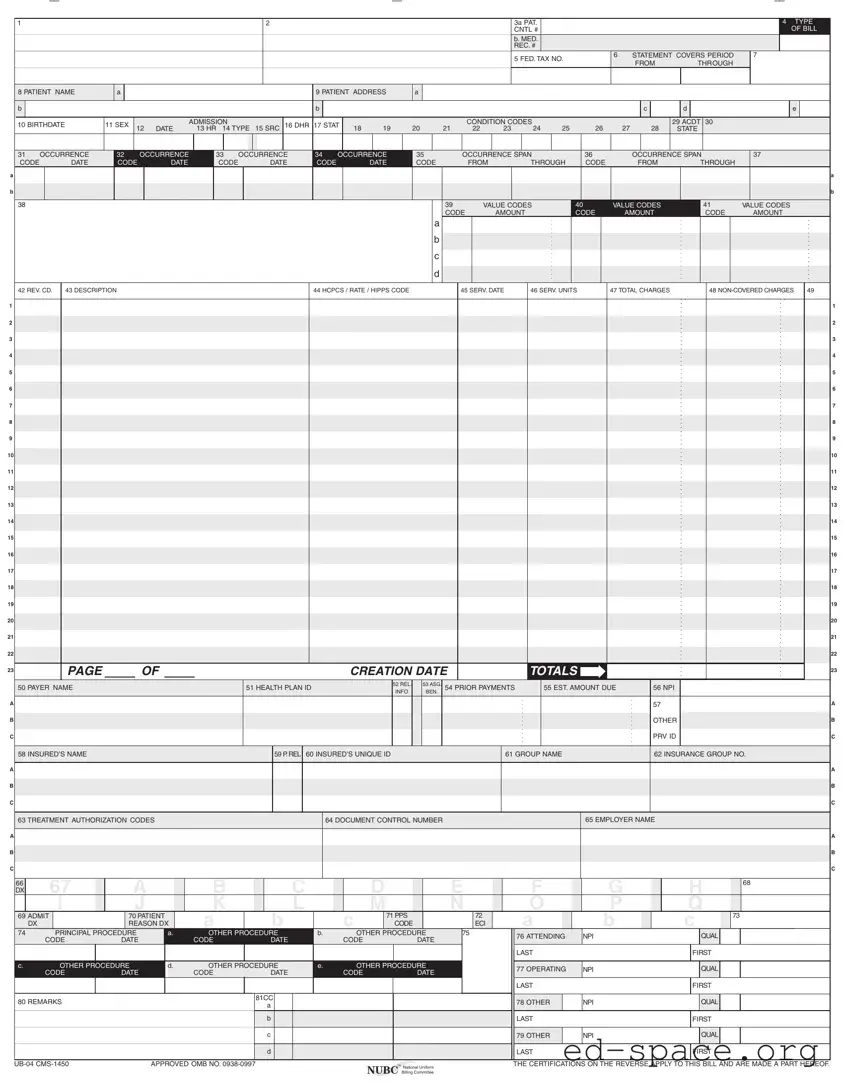
Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS
Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS
Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS
Submission of this claim constitutes certification that the billing
information as shown on the face hereof is true, accurate and complete.
That the submitter did not knowingly or recklessly disregard or
misrepresent or conceal material facts. The following certifications or
verifications apply where pertinent to this Bill:
1. If third party benefits are indicated, the appropriate assignments by
the insured /beneficiary and signature of the patient or parent or a
legal guardian covering authorization to release information are on file.
Determinations as to the release of medical and financial information
should be guided by the patient or the patient’s legal representative.
2. If patient occupied a private room or required private nursing for
medical necessity, any required certifications are on file.
3. Physician’s certifications and re-certifications, if required by contract
or Federal regulations, are on file.
4. For Religious Non-Medical facilities, verifications and if necessary re-
certifications of the patient’s need for services are on file.
5. Signature of patient or his representative on certifications,
authorization to release information, and payment request, as
required by Federal Law and Regulations (42 USC 1935f, 42 CFR
424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other
applicable contract regulations, is on file.
6. The provider of care submitter acknowledges that the bill is in
conformance with the Civil Rights Act of 1964 as amended. Records
adequately describing services will be maintained and necessary
information will be furnished to such governmental agencies as
required by applicable law.
7. For Medicare Purposes: If the patient has indicated that other health
insurance or a state medical assistance agency will pay part of
his/her medical expenses and he/she wants information about
his/her claim released to them upon request, necessary authorization
is on file. The patient’s signature on the provider’s request to bill
Medicare medical and non-medical information, including
employment status, and whether the person has employer group
health insurance which is responsible to pay for the services for
which this Medicare claim is made.
8. For Medicaid purposes: The submitter understands that because
payment and satisfaction of this claim will be from Federal and State
funds, any false statements, documents, or concealment of a
material fact are subject to prosecution under applicable Federal or
State Laws.
9. For TRICARE Purposes:
(a) The information on the face of this claim is true, accurate and
complete to the best of the submitter’s knowledge and belief, and
services were medically necessary and appropriate for the health
of the patient;
(b) The patient has represented that by a reported residential address
outside a military medical treatment facility catchment area he or
she does not live within the catchment area of a U.S. military
medical treatment facility, or if the patient resides within a
catchment area of such a facility, a copy of Non-Availability
Statement (DD Form 1251) is on file, or the physician has certified
to a medical emergency in any instance where a copy of a Non-
Availability Statement is not on file;
(c) The patient or the patient’s parent or guardian has responded
directly to the provider’s request to identify all health insurance
coverage, and that all such coverage is identified on the face of
the claim except that coverage which is exclusively supplemental
payments to TRICARE-determined benefits;
(d) The amount billed to TRICARE has been billed after all such
coverage have been billed and paid excluding Medicaid, and the
amount billed to TRICARE is that remaining claimed against
TRICARE benefits;
(e) The beneficiary’s cost share has not been waived by consent or
failure to exercise generally accepted billing and collection efforts;
and,
(f) Any hospital-based physician under contract, the cost of whose
services are allocated in the charges included in this bill, is not an
employee or member of the Uniformed Services. For purposes of
this certification, an employee of the Uniformed Services is an
employee, appointed in civil service (refer to 5 USC 2105),
including part-time or intermittent employees, but excluding
contract surgeons or other personal service contracts. Similarly,
member of the Uniformed Services does not apply to reserve
members of the Uniformed Services not on active duty.
(g) Based on 42 United States Code 1395cc(a)(1)(j) all providers
participating in Medicare must also participate in TRICARE for
inpatient hospital services provided pursuant to admissions to
hospitals occurring on or after January 1, 1987; and
(h) If TRICARE benefits are to be paid in a participating status, the
submitter of this claim agrees to submit this claim to the
appropriate TRICARE claims processor. The provider of care
submitter also agrees to accept the TRICARE determined
reasonable charge as the total charge for the medical services or
supplies listed on the claim form. The provider of care will accept
the TRICARE-determined reasonable charge even if it is less
than the billed amount, and also agrees to accept the amount
paid by TRICARE combined with the cost-share amount and
deductible amount, if any, paid by or on behalf of the patient as
full payment for the listed medical services or supplies. The
provider of care submitter will not attempt to collect from the
patient (or his or her parent or guardian) amounts over the
TRICARE determined reasonable charge. TRICARE will make
any benefits payable directly to the provider of care, if the
provider of care is a participating provider.
UB-04 NOTICE: THE SUBMITTER OF THIS FORM UNDERSTANDS THAT MISREPRESENTATION OR FALSIFICATION
OF ESSENTIAL INFORMATION AS REQUESTED BY THIS FORM, MAY SERVE AS THE BASIS FOR
CIVIL MONETARTY PENALTIES AND ASSESSMENTS AND MAY UPON CONVICTION INCLUDE
FINES AND/OR IMPRISONMENT UNDER FEDERAL AND/OR STATE LAW(S).
SEE http://www.nubc.org/ FOR MORE INFORMATION ON UB-04 DATA ELEMENT AND PRINTING SPECIFICATIONS