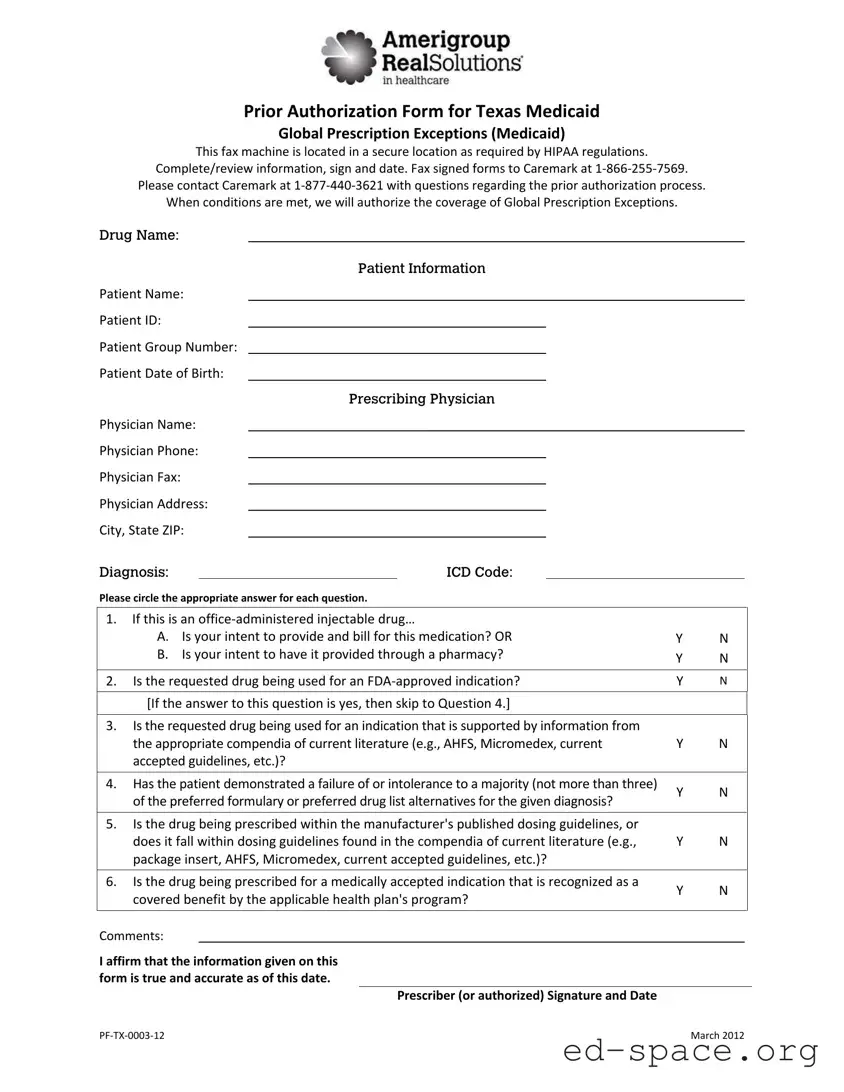
PF‐TX‐0003‐12 March2012
PriorAuthorizationFormforTexasMedicaid
GlobalPrescriptionExceptions(Medicaid)
ThisfaxmachineislocatedinasecurelocationasrequiredbyHIPAAregulations.
Complete/reviewinformation,signanddate.FaxsignedformstoCaremarkat1‐866‐255‐7569.
PleasecontactCaremarkat1‐877‐440‐3621withquestionsregardingthepriorauthorizationprocess.
Whenconditionsaremet,wewillauthorizethecoverageofGlobalPrescriptionExceptions.
Drug Name:
Patient Information
PatientName:
PatientID:
PatientGroupNumber:
PatientDateofBirth:
Prescribing Physician
PhysicianName:
PhysicianPhone:
PhysicianFax:
PhysicianAddress:
City,StateZIP:
Diagnosis:
ICD Code:
Pleasecircletheappropriateanswerforeachquestion.
1. Ifthisisanoffice‐administeredinjectabledrug…
A. Isyourintenttoprovideandbillforthismedication?OR
B. Isyourintenttohaveitprovidedthroughapharmacy?
Y N
Y N
2. IstherequesteddrugbeingusedforanFDA‐approvedindication? Y
N
[Iftheanswertothisquestionisyes,thenskiptoQuestion4.]
3. Istherequesteddrugbeingusedforanindicationthatissupportedbyinformationfrom
theappropriatecompendiaofcurrentliterature(e.g.,AHFS,Micromedex,current
acceptedguidelines,etc.)?
Y N
4. Hasthepatientdemonstratedafailureoforintolerancetoamajority(notmorethanthree)
ofthepreferredformularyorpreferreddruglistalternativesforthegivendiagnosis?
Y N
5. Isthedrugbeingprescribedwithinthemanufacturer'spublisheddosingguidelines,or
doesitfallwithindosingguidelinesfoundinthecompendiaofcurrentliterature(e.g.,
packageinsert,AHFS,Micromedex,currentacceptedguidelines,etc.)?
Y N
6. Isthedrugbeingprescribedforamedicallyacceptedindicationthatisrecognizedasa
coveredbenefitbytheapplicablehealthplan'sprogram?
Y N
Comments:
Iaffirmthattheinformationgivenonthis
formistrueandaccurateasofthisdate.
Prescriber(orauthorized)SignatureandDate