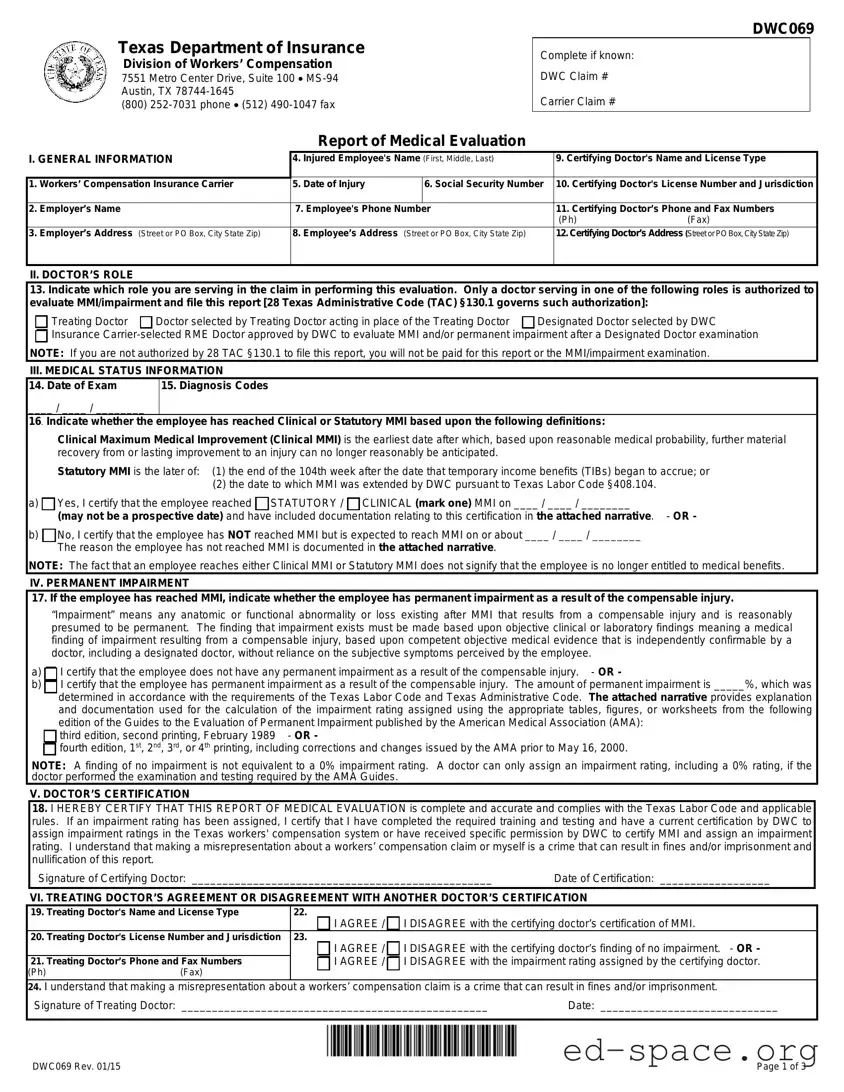
DWC069
DWC069 Rev. 01/15 Page 1 of 3
Texas Department of Insurance
Division of Workers’ Compensation
7551 Metro Center Drive, Suite 100 MS-94
Austin, TX 78744-1645
(800) 252-7031 phone (512) 490-1047 fax
Complete if known:
DWC Claim #
Carrier Claim #
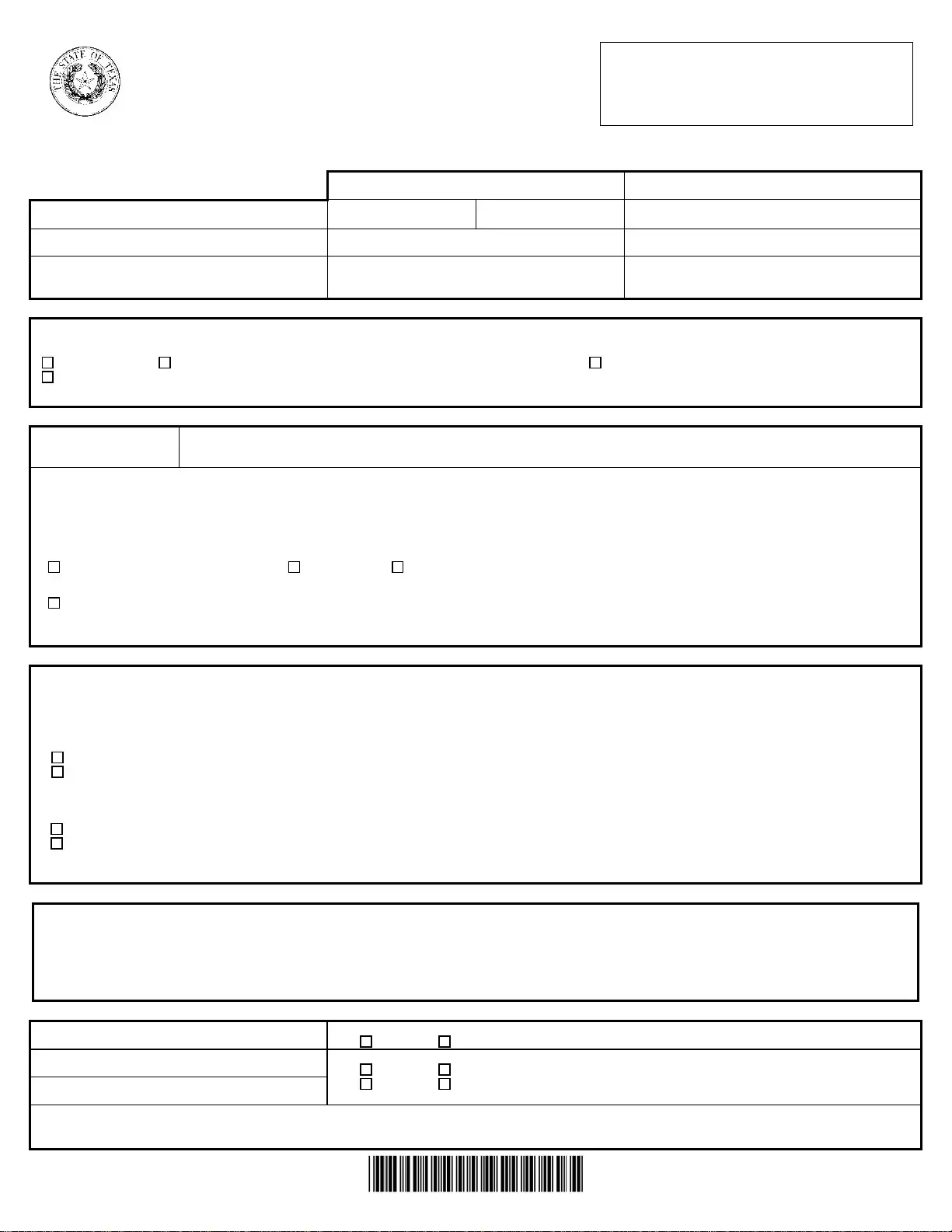
Report of Medical Evaluation
I. GENERAL INFORMATION
4. Injured Employee's Name (First, Middle, Last)
9. Certifying Doctor's Name and License Type
1. Workers’ Compensation Insurance Carrier
5. Date of Injury
6. Social Security Number
10. Certifying Doctor's License Number and Jurisdiction
2. Employer’s Name
7. Employee's Phone Number 11. Certifying Doctor’s Phone and Fax Numbers
(Ph) (Fax)
3. Employer’s Address (Street or PO Box, City State Zip)
8. Employee’s Address (Street or PO Box, City State Zip) 12. Certifying Doctor’s Address (Street or PO Box, City State Zip)
II. DOCTOR’S ROLE
13. Indicate which role you are serving in the claim in performing this evaluation. Only a doctor serving in one of the following roles is authorized to
evaluate MMI/impairment and file this report [28 Texas Administrative Code (TAC) §130.1 governs such authorization]:
Treating Doctor Doctor selected by Treating Doctor acting in place of the Treating Doctor Designated Doctor selected by DWC
Insurance Carrier-selected RME Doctor approved by DWC to evaluate MMI and/or permanent impairment after a Designated Doctor examination
NOTE: If you are not authorized by 28 TAC §130.1 to file this report, you will not be paid for this report or the MMI/impairment examination.
III. MEDICAL STATUS INFORMATION
14. Date of Exam
____ / ____ / ________
15. Diagnosis Codes
16. Indicate whether the employee has reached Clinical or Statutory MMI based upon the following definitions:
Clinical Maximum Medical Improvement (Clinical MMI) is the earliest date after which, based upon reasonable medical probability, further material
recovery from or lasting improvement to an injury can no longer reasonably be anticipated.
Statutory MMI is the later of: (1) the end of the 104th week after the date that temporary income benefits (TIBs) began to accrue; or
(2) the date to which MMI was extended by DWC pursuant to Texas Labor Code §408.104.
a) Yes, I certify that the employee reached STATUTORY / CLINICAL (mark one) MMI on ____ / ____ / ________
(may not be a prospective date) and have included documentation relating to this certification in the attached narrative. - OR -
b) No, I certify that the employee has NOT reached MMI but is expected to reach MMI on or about ____ / ____ / ________
The reason the employee has not reached MMI is documented in the attached narrative.
NOTE: The fact that an employee reaches either Clinical MMI or Statutory MMI does not signify that the employee is no longer entitled to medical benefits.
IV. PERMANENT IMPAIRMENT
17. If the employee has reached MMI, indicate whether the employee has permanent impairment as a result of the compensable injury.
“Impairment” means any anatomic or functional abnormality or loss existing after MMI that results from a compensable injury and is reasonably
presumed to be permanent. The finding that impairment exists must be made based upon objective clinical or laboratory findings meaning a medical
finding of impairment resulting from a compensable injury, based upon competent objective medical evidence that is independently confirmable by a
doctor, including a designated doctor, without reliance on the subjective symptoms perceived by the employee.
a) I certify that the employee does not have any permanent impairment as a result of the compensable injury. - OR -
b) I certify that the employee has permanent impairment as a result of the compensable injury. The amount of permanent impairment is _____%, which was
determined in accordance with the requirements of the Texas Labor Code and Texas Administrative Code. The attached narrative provides explanation
and documentation used for the calculation of the impairment rating assigned using the appropriate tables, figures, or worksheets from the following
edition of the Guides to the Evaluation of Permanent Impairment published by the American Medical Association (AMA):
third edition, second printing, February 1989 - OR -
fourth edition, 1
st
, 2
nd
, 3
rd
, or 4
th
printing, including corrections and changes issued by the AMA prior to May 16, 2000.
NOTE: A finding of no impairment is not equivalent to a 0% impairment rating. A doctor can only assign an impairment rating, including a 0% rating, if the
doctor
erformed the examination and testin
re
uired b
the AMA Guides.
V. DOCTOR’S CERTIFICATION
18. I HEREBY CERTIFY THAT THIS REPORT OF MEDICAL EVALUATION is complete and accurate and complies with the Texas Labor Code and applicable
rules. If an impairment rating has been assigned, I certify that I have completed the required training and testing and have a current certification by DWC to
assign impairment ratings in the Texas workers' compensation system or have received specific permission by DWC to certify MMI and assign an impairment
rating. I understand that making a misrepresentation about a workers’ compensation claim or myself is a crime that can result in fines and/or imprisonment and
nullification of this report.
Signature of Certifying Doctor: _________________________________________________ Date of Certification: __________________
VI. TREATING DOCTOR’S AGREEMENT OR DISAGREEMENT WITH ANOTHER DOCTOR’S CERTIFICATION
19. Treating Doctor's Name and License Type
22.
I AGREE / I DISAGREE with the certifying doctor’s certification of MMI.
20. Treating Doctor's License Number and Jurisdiction 23.
I AGREE / I DISAGREE with the certifying doctor’s finding of no impairment. - OR -
I AGREE / I DISAGREE with the impairment rating assigned by the certifying doctor.
21. Treating Doctor’s Phone and Fax Numbers
(Ph) (Fax)
24. I understand that making a misrepresentation about a workers’ compensation claim is a crime that can result in fines and/or imprisonment.
Signature of Treating Doctor: __________________________________________________ Date: _____________________________