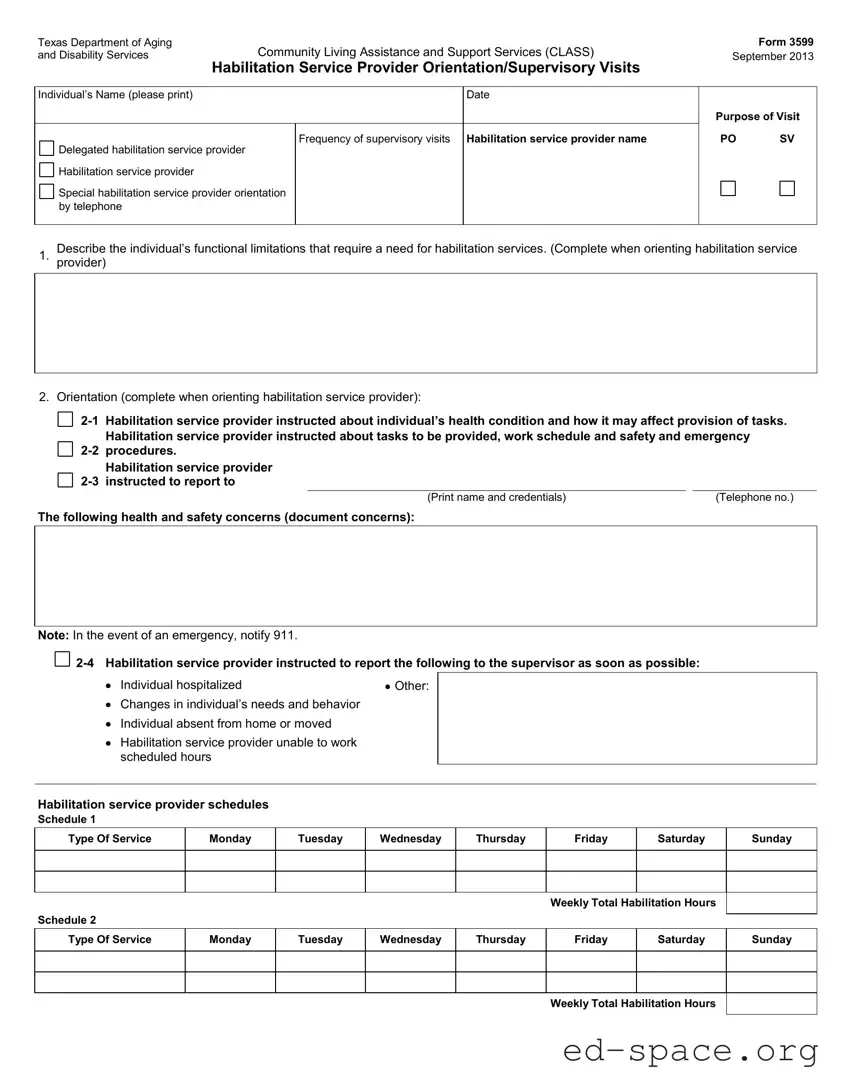
What is the purpose of the Texas 3599 form?
The Texas 3599 form is used for documenting supervisory visits and orientations for habilitation service providers. It helps ensure that providers are properly informed about the individual’s health conditions, needs, and the tasks they are expected to perform. This form is crucial for maintaining quality care and support for individuals receiving habilitation services.
Who should fill out the Texas 3599 form?
The form should be completed by the habilitation service provider during supervisory visits. It may also involve input from the individual receiving services or their legally authorized representative (LAR). Accurate information is essential for assessing the effectiveness of the services provided and ensuring the individual’s needs are met.
What information is required on the Texas 3599 form?
Key information includes the individual's name, date of the visit, frequency of visits, and details about the habilitation service provider. The form also requires documentation of the individual’s functional limitations, health concerns, and any changes in needs or behavior. Additionally, it captures the tasks performed by the provider and the individual’s satisfaction with the services.
How often should the Texas 3599 form be completed?
The Texas 3599 form should be completed during each supervisory visit. The frequency of these visits may vary based on individual needs and the service provider's schedule. Regular documentation helps track progress and ensures that the care provided remains appropriate and effective.
What should be done if there are issues with service delivery?
If there are any service delivery problems, they must be documented on the Texas 3599 form. This includes describing the issues and identifying any training needs for the habilitation service provider. Corrective actions should also be noted to ensure that necessary improvements are made to enhance the quality of care.
What happens after the Texas 3599 form is completed?
Once the Texas 3599 form is completed, it should be signed by the individual or their LAR, the habilitation service provider, and the supervisor. This signature process confirms that all parties are aware of the information documented. The completed form is then kept on file for future reference and review, ensuring continuity of care.