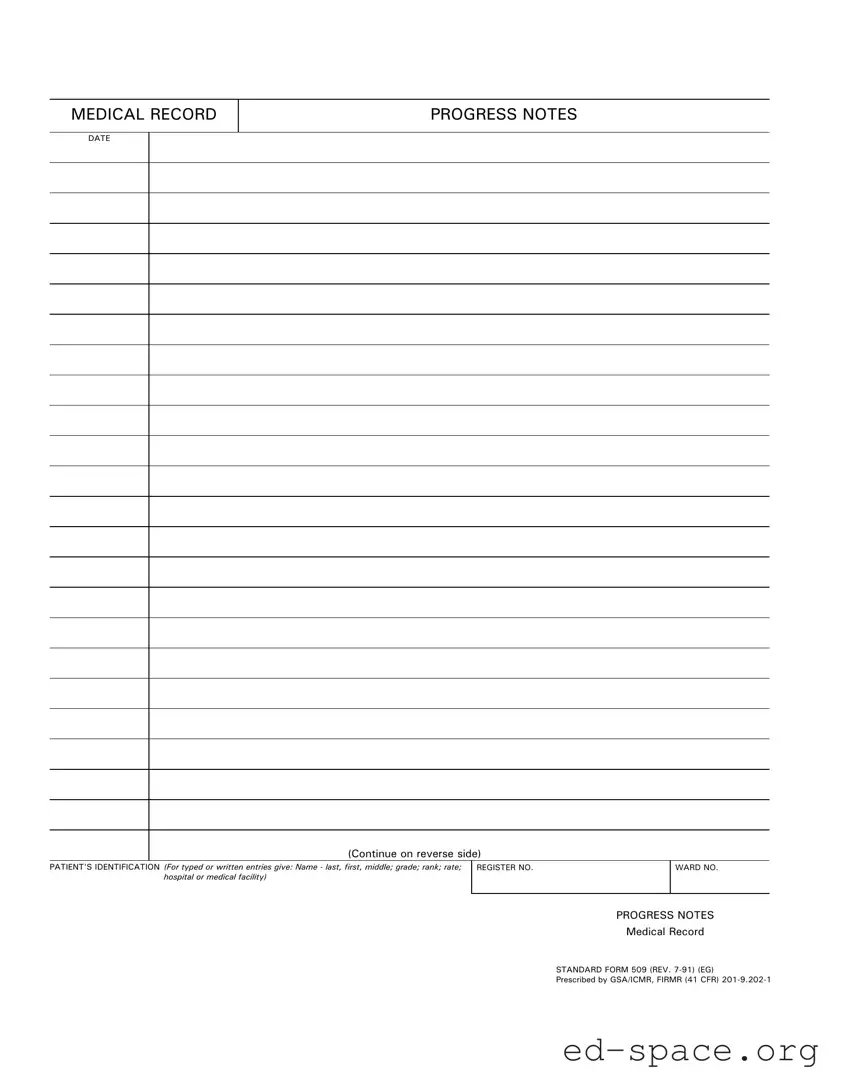
What is the purpose of the Progress Notes form?
The Progress Notes form is used to document a patient's medical history, treatment, and progress during their stay in a medical facility. It provides a structured way for healthcare providers to record observations, changes in condition, and any interventions performed. This documentation is crucial for maintaining accurate medical records and ensuring continuity of care.
What information is required on the Progress Notes form?
The form requires specific patient identification details, including the patient's name (last, first, middle), grade, rank, rate, and the name of the hospital or medical facility. Additionally, the date of the entry must be included. These details help to ensure that the records are correctly attributed to the right patient.
How should the Progress Notes be filled out?
Entries on the Progress Notes form can be made either by typing or writing. It is important to provide clear and legible information to avoid any misunderstandings. Each entry should be dated and should reflect the patient's current status, treatment provided, and any relevant observations made by the healthcare provider.
Is there a specific format to follow for the Progress Notes?
While the Progress Notes form is standardized, the actual content can vary based on the patient's condition and the healthcare provider's observations. Providers should follow any specific guidelines set by their medical facility regarding the format and detail of the notes. Consistency in documentation is key to effective communication among care teams.
What should be done if additional space is needed on the form?
If more space is needed for additional notes, healthcare providers are encouraged to continue writing on the reverse side of the form. This allows for comprehensive documentation without losing important information. It is essential to ensure that all entries are clearly marked and dated.
Who has access to the Progress Notes?
Access to the Progress Notes is typically limited to authorized healthcare personnel involved in the patient's care. This includes doctors, nurses, and other relevant staff. Patient confidentiality must be maintained at all times, in accordance with privacy regulations.
How often should Progress Notes be updated?
Progress Notes should be updated regularly, especially after any significant changes in the patient's condition or after treatment interventions. Frequent updates ensure that all members of the healthcare team have the most current information, which is vital for effective patient care.