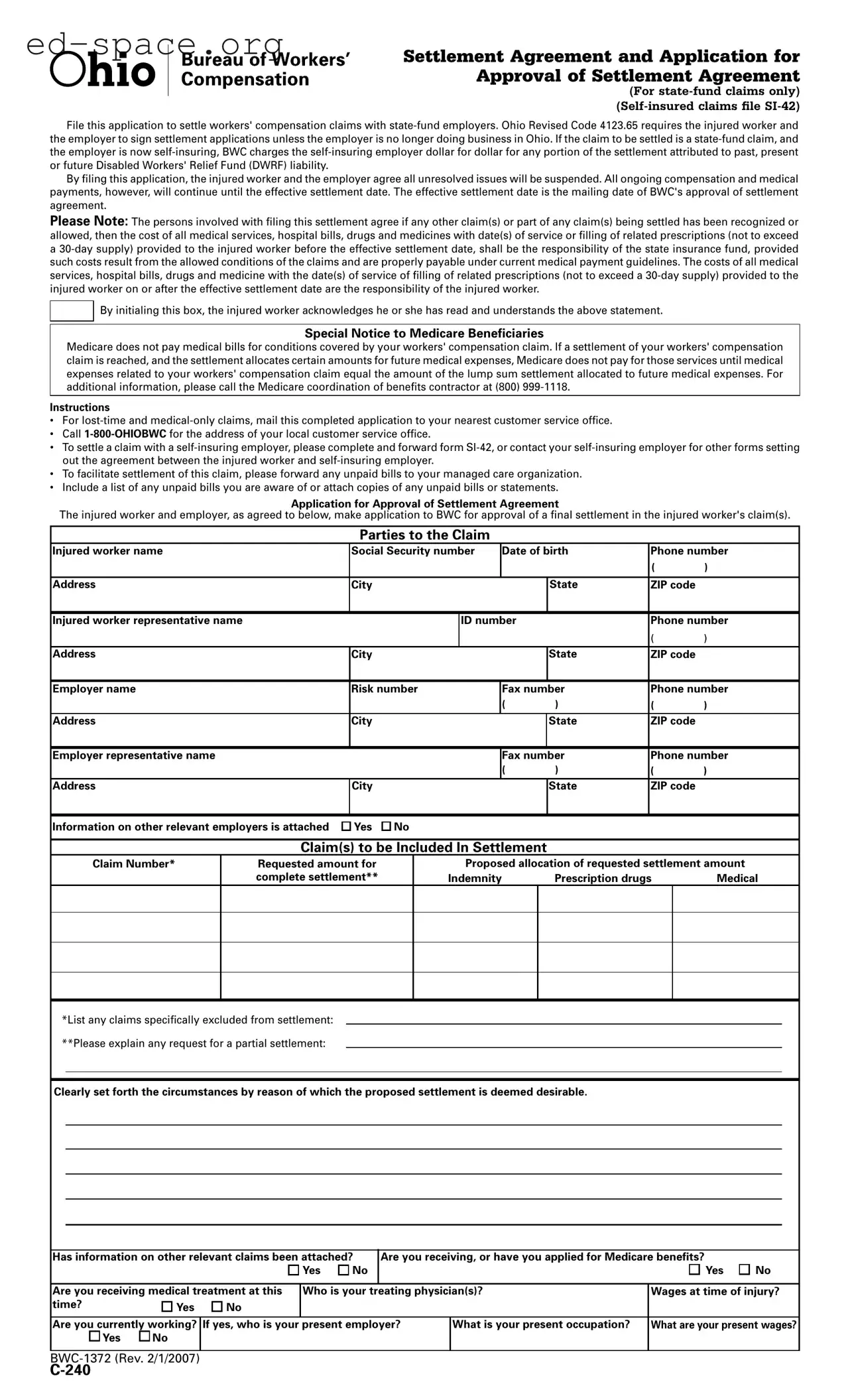
Settlement Agreement and Application for
Approval of Settlement Agreement
(For state-fund claims only) (Self-insured claims file SI-42)
File this application to settle workers' compensation claims with state-fund employers. Ohio Revised Code 4123.65 requires the injured worker and the employer to sign settlement applications unless the employer is no longer doing business in Ohio. If the claim to be settled is a state-fund claim, and the employer is now self-insuring, BWC charges the self-insuring employer dollar for dollar for any portion of the settlement attributed to past, present or future Disabled Workers' Relief Fund (DWRF) liability.
By iling this application, the injured worker and the employer agree all unresolved issues will be suspended. All ongoing compensation and medical payments, however, will continue until the effective settlement date. The effective settlement date is the mailing date of BWC's approval of settlement agreement.
Please Note: The persons involved with iling this settlement agree if any other claim(s) or part of any claim(s) being settled has been recognized or allowed, then the cost of all medical services, hospital bills, drugs and medicines with date(s) of service or illing of related prescriptions (not to exceed a 30-day supply) provided to the injured worker before the effective settlement date, shall be the responsibility of the state insurance fund, provided such costs result from the allowed conditions of the claims and are properly payable under current medical payment guidelines. The costs of all medical services, hospital bills, drugs and medicine with the date(s) of service of illing of related prescriptions (not to exceed a 30-day supply) provided to the injured worker on or after the effective settlement date are the responsibility of the injured worker.
By initialing this box, the injured worker acknowledges he or she has read and understands the above statement.
Special Notice to Medicare Beneficiaries
Medicare does not pay medical bills for conditions covered by your workers' compensation claim. If a settlement of your workers' compensation claim is reached, and the settlement allocates certain amounts for future medical expenses, Medicare does not pay for those services until medical expenses related to your workers' compensation claim equal the amount of the lump sum settlement allocated to future medical expenses. For additional information, please call the Medicare coordination of beneits contractor at (800) 999-1118.
Instructions
•For lost-time and medical-only claims, mail this completed application to your nearest customer service ofice.
•Call 1-800-OHIOBWC for the address of your local customer service ofice.
•To settle a claim with a self-insuring employer, please complete and forward form SI-42, or contact your self-insuring employer for other forms setting out the agreement between the injured worker and self-insuring employer.
•To facilitate settlement of this claim, please forward any unpaid bills to your managed care organization.
•Include a list of any unpaid bills you are aware of or attach copies of any unpaid bills or statements.
Application for Approval of Settlement Agreement
The injured worker and employer, as agreed to below, make application to BWC for approval of a inal settlement in the injured worker's claim(s).
Parties to the Claim
Injured worker name |
Social Security number |
Date of birth |
Phone number |
|
|
|
|
|
|
( |
) |
|
|
|
|
|
|
|
|
Address |
City |
|
|
|
State |
ZIP code |
|
|
|
|
|
|
|
|
Injured worker representative name |
|
|
ID number |
|
Phone number |
|
|
|
|
|
|
( |
) |
Address |
City |
|
|
|
State |
ZIP code |
|
|
|
|
|
|
|
Employer name |
Risk number |
Fax number |
Phone number |
|
|
|
|
( |
) |
( |
) |
Address |
City |
|
|
|
State |
ZIP code |
|
|
|
|
|
|
|
|
Employer representative name |
|
|
|
Fax number |
Phone number |
|
|
|
|
( |
) |
( |
) |
Address |
City |
|
|
|
State |
ZIP code |
|
|
|
|
|
|
|
|
|
Information on other relevant employers is attached |
Yes |
No |
|
|
|
|
Claim(s) to be Included In Settlement
|
Claim Number* |
Requested amount for |
|
|
Proposed allocation of requested settlement amount |
|
|
|
|
|
|
complete settlement** |
|
Indemnity |
Prescription drugs |
Medical |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
*List any claims speciically excluded from settlement: |
|
|
|
|
|
|
|
|
|
|
**Please explain any request for a partial settlement: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Clearly set forth the circumstances by reason of which the proposed settlement is deemed desirable. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Has information on other relevant claims been attached? |
Are you receiving, or have you applied for Medicare benefits? |
|
|
|
|
|
|
|
|
Yes |
No |
|
|
|
|
|
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
Are you receiving medical treatment at this |
Who is your treating physician(s)? |
|
Wages at time of injury? |
time? |
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Are you currently working? |
If yes, who is your present employer? |
|
What is your present occupation? |
What are your present wages? |
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
BWC-1372 (Rev. 2/1/2007)