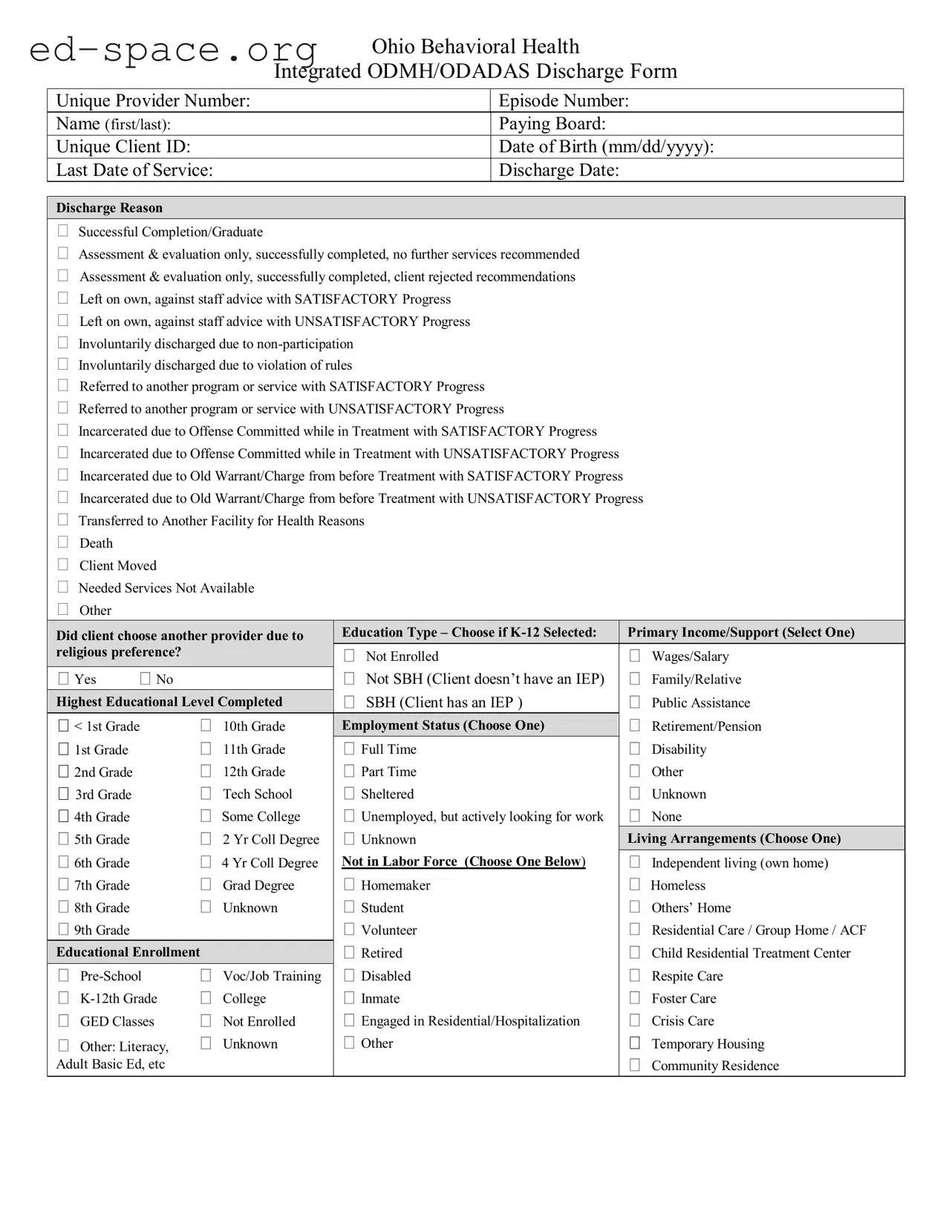
What is the Ohio Behavioral Discharge form?
The Ohio Behavioral Discharge form is a document used to record the details of a client’s discharge from behavioral health services. It captures essential information, including the client's unique identifiers, discharge reasons, and relevant health and social data. This form is crucial for ensuring that all parties involved in the client’s care have a clear understanding of their treatment journey and discharge status.
Who needs to fill out the Ohio Behavioral Discharge form?
The form must be completed by the provider or staff member responsible for the client's care at the time of discharge. This includes therapists, case managers, or any authorized personnel who have been involved in the client's treatment process. Accurate completion is vital to ensure continuity of care and proper documentation.
What information is required on the form?
Essential information includes the client's name, unique client ID, date of birth, last date of service, and discharge date. Additionally, the form requires the reason for discharge, which can range from successful completion to involuntary discharge due to non-participation. Other sections address the client's educational background, living arrangements, and health conditions.
What are the possible discharge reasons listed on the form?
The form includes various discharge reasons such as successful completion of treatment, assessment and evaluation only, voluntary departure against staff advice, involuntary discharge due to rule violations, and referrals to other services. Each reason is critical for understanding the client's progress and future needs.
How does the form address the client's educational background?
The form includes sections for recording the highest educational level completed by the client and their current educational enrollment status. This information helps providers understand the client’s background and tailor future services accordingly.
What is the significance of the drug of choice section?
This section allows providers to document the client’s primary, secondary, and tertiary substances of abuse. Understanding the client's drug history is crucial for developing effective treatment plans and ensuring appropriate follow-up care.
How is the form used for future service planning?
The information collected on the Ohio Behavioral Discharge form is instrumental in planning future services for the client. By capturing discharge reasons, health conditions, and social determinants, providers can make informed decisions about referrals and ongoing support that may be necessary for the client’s recovery journey.
What happens to the form after it is completed?
Once the form is completed, it is typically stored in the client's medical record. It may also be shared with relevant stakeholders involved in the client's care, such as other treatment facilities or support services, to ensure a smooth transition and continuity of care.
Where can I obtain the Ohio Behavioral Discharge form?
The Ohio Behavioral Discharge form can usually be obtained from the Ohio Department of Mental Health and Addiction Services website or directly from behavioral health providers. It is important to ensure that you have the most current version of the form to comply with state requirements.