What is the purpose of the Michigan Molina Prior Authorization form?
The Michigan Molina Prior Authorization form is used to request approval for specific medical services before they are provided. This process ensures that the requested services are medically necessary and covered under the member's plan. It helps streamline care and ensures that members receive appropriate treatments in a timely manner.
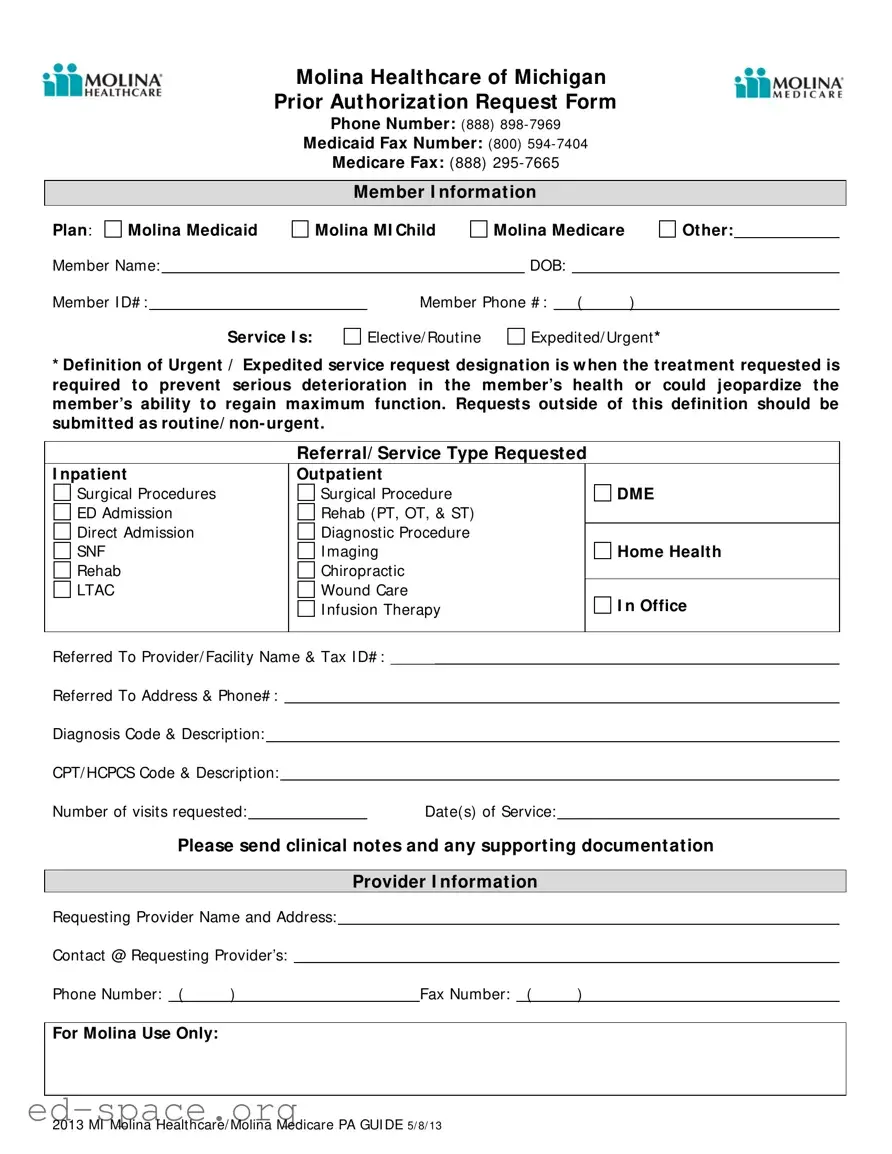
How do I submit the Prior Authorization request?
You can submit the Prior Authorization request by completing the form and sending it via fax. For Medicaid requests, use the fax number (800) 594-7404. For Medicare requests, send it to (888) 295-7665. Ensure that you include all required information, including diagnosis codes and supporting documentation, to avoid delays in processing.
What types of services require Prior Authorization?
Prior Authorization is typically required for various services such as inpatient and outpatient procedures, surgical procedures, diagnostic tests, and certain therapies like physical or occupational therapy. It is crucial to determine whether the service is elective/routine or urgent/expedited. Urgent requests must meet specific criteria to be considered for expedited review.
What information do I need to provide on the form?
When filling out the form, you must provide detailed information, including the member's name, ID number, date of birth, and contact information. Additionally, specify the type of service requested, diagnosis codes, CPT/HCPCS codes, and the number of visits needed. Don't forget to include clinical notes and any other supporting documentation to ensure a smooth approval process.