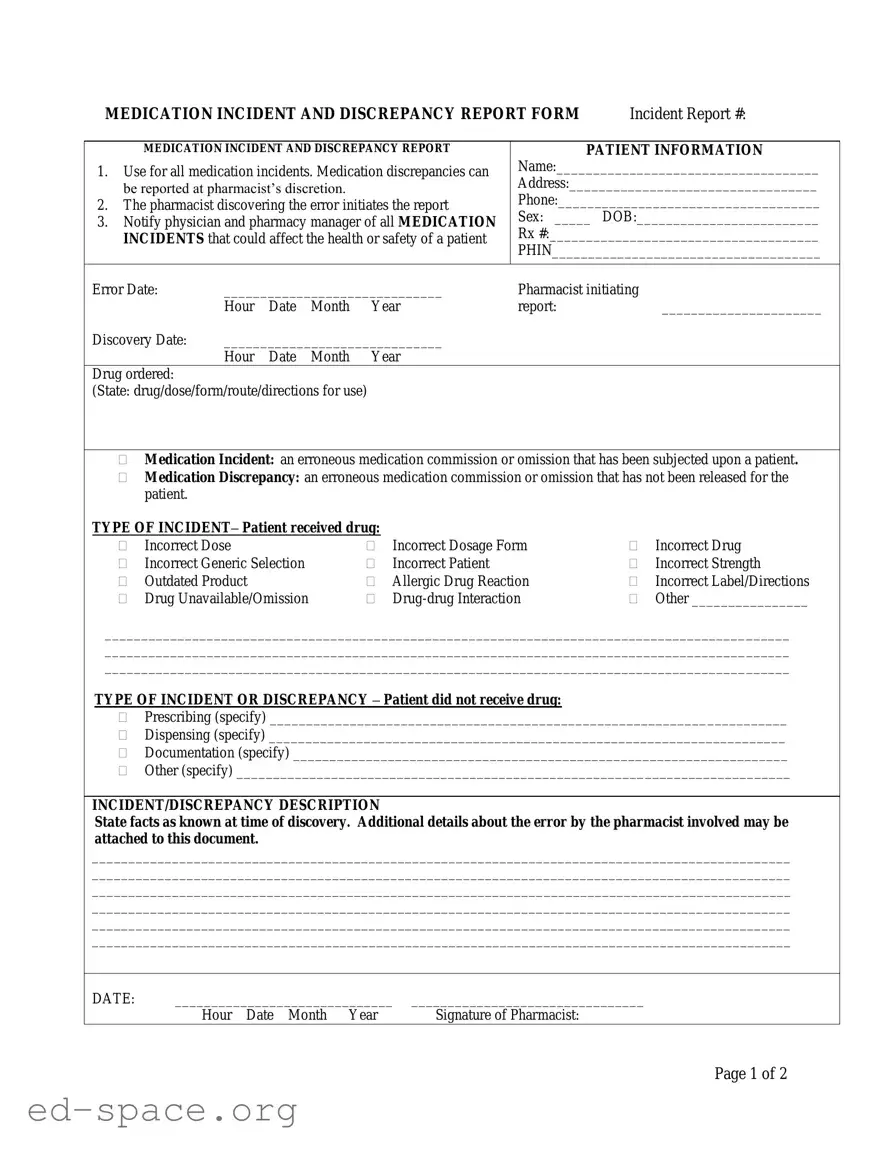
What is the purpose of the Medication Error form?
The Medication Error form is designed to report any incidents or discrepancies related to medication. This includes both medication incidents, where a patient has received the wrong medication or dosage, and medication discrepancies, where an error occurred but the medication was not yet administered to the patient. The form helps ensure patient safety and allows for proper documentation and follow-up.
Who should initiate the Medication Error report?
The pharmacist who discovers the medication error is responsible for initiating the report. This ensures that the person with the most knowledge of the incident provides accurate information for the report.
What should be included in the incident description?
The incident description should include all known facts at the time of discovery. It is important to provide detailed information about the error, including what happened, how it happened, and any immediate actions taken. Additional details can be attached to the form if necessary.
What steps should be taken after a medication incident is reported?
After a medication incident is reported, the pharmacist must notify both the physician and the pharmacy manager. This notification is crucial for ensuring that the patient’s health and safety are prioritized and that appropriate follow-up actions can be taken.
What types of incidents can be reported using this form?
The form can be used to report various types of medication incidents, including incorrect doses, incorrect drugs, allergic reactions, and drug-drug interactions, among others. It can also document discrepancies, such as prescribing or dispensing errors.
What information is required for patient notification?
When notifying the patient about a medication incident, the report must include the date and time of notification. This ensures that there is a clear record of communication regarding the incident and any potential impacts on the patient’s health.
How is the severity of the incident assessed?
The severity of the incident is assessed based on the impact on the patient’s condition. The form includes categories ranging from no change in condition to incidents requiring immediate medical intervention. This assessment helps determine the necessary follow-up actions and educational needs.