What is a Medication Administration Record Sheet?
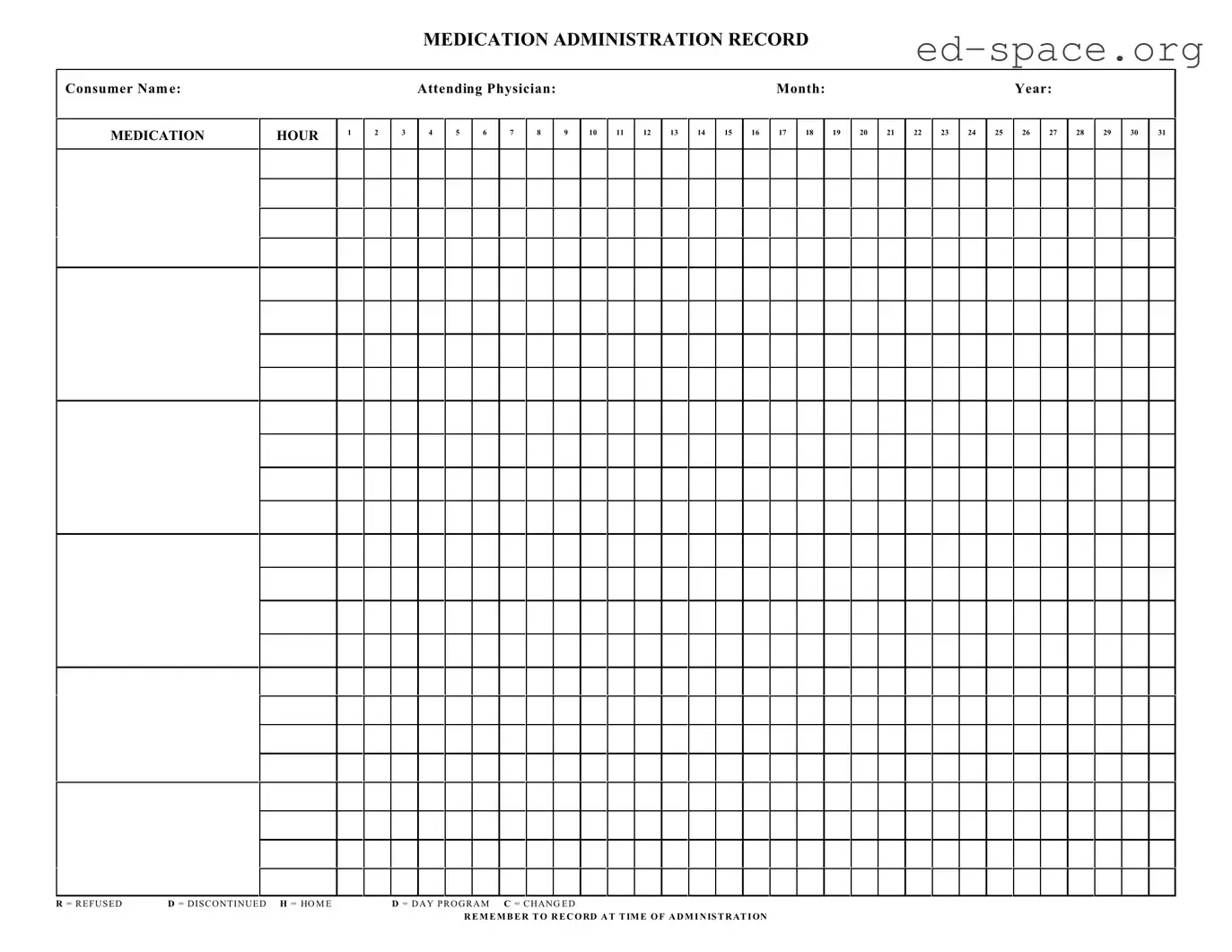
A Medication Administration Record Sheet is a document used to track the administration of medications to an individual over a specific period of time. This sheet records essential details such as the name of the person receiving medication, the type of medication, dosage, the time medication is taken, and any notes related to changes in medication, refusal of medication, or medication taken while away from home or in a day program.
Who needs to use a Medication Administration Record Sheet?
This form is typically used by caregivers, healthcare professionals, and facilities that provide care to individuals requiring assistance with medication management. It is especially useful in settings where multiple individuals are responsible for administering medications, such as in senior care facilities, hospitals, or in home care scenarios.
Why is it important to record medication administration?
Recording medication administration is crucial for ensuring the safety and well-being of the individual receiving care. It helps in monitoring dosage accuracy, timing of medication, and identifying any side effects or adverse reactions. This record also facilitates communication among caregivers and healthcare professionals, making it easier to track the effectiveness of medications and make necessary adjustments.
How should the Medication Administration Record Sheet be filled out?
When filling out the sheet, it's important to write legibly and include all relevant details such as the consumer's name, the medication name, the dosage, and the specific time of administration. Any changes in medication, instances where medication is refused, or when medication is taken while away from the usual care setting should be clearly noted using the designated symbols (R for refused, D for discontinued, H for home, D for day program, C for changed).
Can this sheet be used for multiple months?
No, the Medication Administration Record Sheet is designed for use over a single month. Each month requires a new form to ensure accurate and up-to-date recording of medication administration. This monthly approach helps in effective monitoring and management of the individual's medication regimen.
What should be done if a medication is refused or discontinued?
Any instances where medication is refused by the individual or discontinued by the attending physician should be immediately recorded on the sheet using the appropriate symbol (R for refused, D for discontinued). Additional notes detailing the reason for refusal or discontinuation and the date of occurrence should also be included. This information is critical for healthcare providers to review and take necessary actions.
How is medication administered outside of the home or in a day program documented?
Medication administered outside of the usual care setting, such as in a day program or while the individual is at home (and not under the direct care of the facility or caregiver), should be documented using the symbols H for home and D for day program. It is important to also record the time of administration and any other relevant details to ensure continuity in the medication management process.
What does the letter C stand for in the medication administration process?
The letter C stands for "Changed" on the Medication Administration Record Sheet. It is used to indicate any changes to the medication regimen, including changes in dosage, frequency, or the medication itself. Detailing these changes on the sheet ensures accurate tracking and helps in assessing the effectiveness of the medication regimen over time.
Is it necessary to record the time of medication administration?
Yes, recording the exact time of medication administration is essential. It ensures that medications are given at the correct intervals, avoids missed or duplicate doses, and helps in monitoring the medication's effectiveness and any potential side effects. This practice is crucial for maintaining the individual's health and safety.
Who should have access to the Medication Administration Record Sheet?
Access to the Medication Administration Record Sheet should be limited to individuals directly involved in the care and medication management of the consumer, such as healthcare professionals, caregivers, and authorized facility staff. It's important to keep this information confidential and secure to protect the privacy and well-being of the individual receiving care.