What is the purpose of the History and Physical (H&P) form?
The History and Physical form serves as a comprehensive document that captures a patient's medical history and current health status. It is essential for healthcare providers to gather detailed information about the patient’s chief complaint, past medical and surgical history, medications, and family background. This information aids in forming an accurate diagnosis and developing an effective treatment plan. The H&P form ensures that all relevant details are recorded systematically, facilitating better communication among medical staff and enhancing patient care.
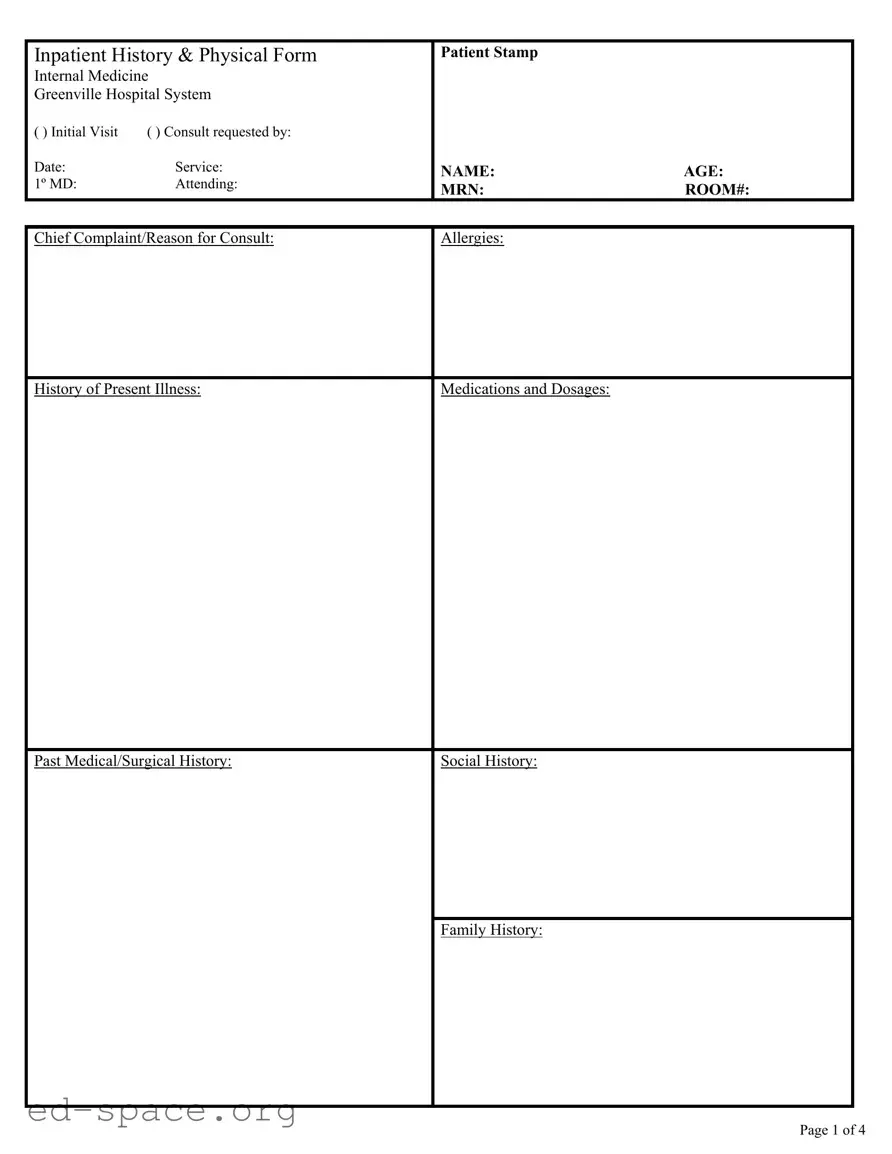
What information is typically included in the H&P form?
The H&P form typically includes several key sections. It starts with basic patient information such as name, age, and medical record number. The form then outlines the chief complaint, allergies, and a detailed history of the present illness. Additionally, it covers past medical and surgical history, medications, social history, and family history. A comprehensive review of systems (ROS) is also included, which examines various body systems to identify any additional health concerns. Finally, the physical exam section records vital signs and findings from the examination, providing a holistic view of the patient's health.
Why is a review of systems (ROS) important in the H&P form?
The review of systems (ROS) is a critical component of the H&P form. It systematically evaluates each body system to uncover any symptoms that may not have been initially reported by the patient. This thorough approach helps healthcare providers identify underlying issues that could impact diagnosis and treatment. By documenting symptoms such as headaches, chest pain, or gastrointestinal issues, providers can ensure that all potential health concerns are addressed, leading to more effective and personalized care.
How does the H&P form assist in patient care and treatment planning?
The H&P form plays a vital role in patient care and treatment planning. By compiling a detailed account of the patient's medical history and current health status, it allows healthcare providers to make informed decisions. The information gathered helps in diagnosing conditions accurately, planning appropriate interventions, and monitoring progress. Furthermore, it serves as a reference for all healthcare team members involved in the patient's care, ensuring continuity and consistency in treatment.
Who is responsible for completing the H&P form?