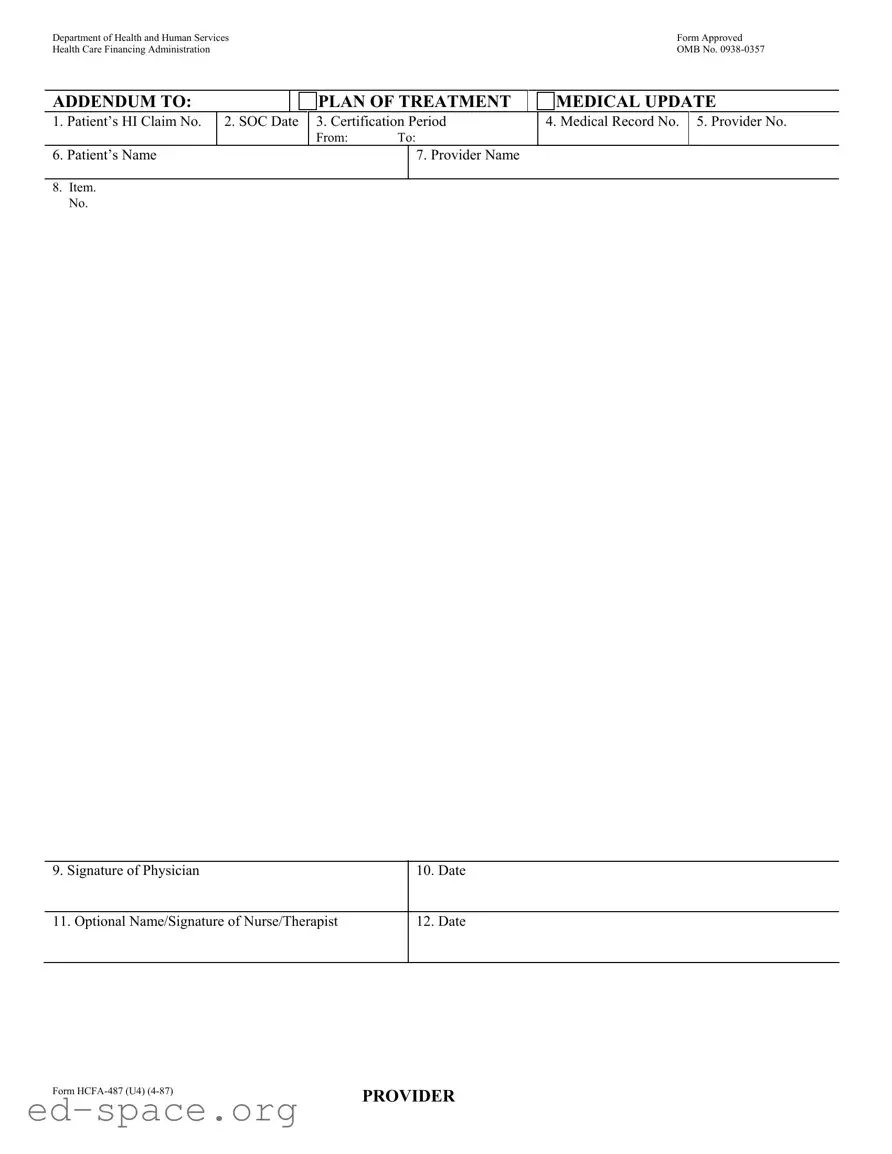
What is the HCFA 487 form used for?
The HCFA 487 form, also known as the Addendum to Plan of Treatment Medical Update, is used to provide updates regarding a patient's treatment plan. It is typically completed by healthcare providers to document changes in a patient’s medical condition or treatment needs. This form is essential for ensuring that all parties involved in a patient’s care are informed of any modifications, thereby facilitating better coordination and continuity of care.
Who is required to fill out the HCFA 487 form?
Healthcare providers, such as physicians, nurses, or therapists, are responsible for completing the HCFA 487 form. The form is generally filled out when there is a need to update the treatment plan due to changes in the patient’s health status or treatment requirements. In some cases, a nurse or therapist may also sign the form to provide additional insights into the patient’s care.
What information is needed to complete the HCFA 487 form?
To complete the HCFA 487 form, several key pieces of information are required. This includes the patient’s Health Insurance (HI) Claim Number, the Start of Care (SOC) date, the certification period, and the medical record number. Additionally, the form requires the patient's name, the provider's name, and the signature of the physician, along with the date of completion. Optional signatures from nurses or therapists may also be included to enhance the documentation.
How does the HCFA 487 form impact patient care?
The HCFA 487 form plays a crucial role in patient care by ensuring that all healthcare providers involved in a patient’s treatment are on the same page. By documenting updates to the treatment plan, the form helps to prevent miscommunication and ensures that the care provided aligns with the patient's current needs. This can lead to improved health outcomes and a more efficient healthcare process overall.
Where can I obtain a copy of the HCFA 487 form?
A copy of the HCFA 487 form can typically be obtained from healthcare facilities that accept Medicare or Medicaid, as they often use this form for billing and documentation purposes. Additionally, it may be available on the official website of the Centers for Medicare & Medicaid Services (CMS) or through healthcare software systems used by providers. If you are unsure where to find it, contacting your healthcare provider's office is a good first step.