What is the purpose of the Express Scripts Prior Authorization form?
The Express Scripts Prior Authorization form is designed for plan members who have been prescribed a medication that requires prior authorization. This form must be completed and submitted to ensure that the medication can be reimbursed through the member's private drug benefit plan. The completion of this form is essential for the approval process, which is based on clinical criteria established by Health Canada and supporting evidence-based protocols.
Who is responsible for completing the Prior Authorization form?
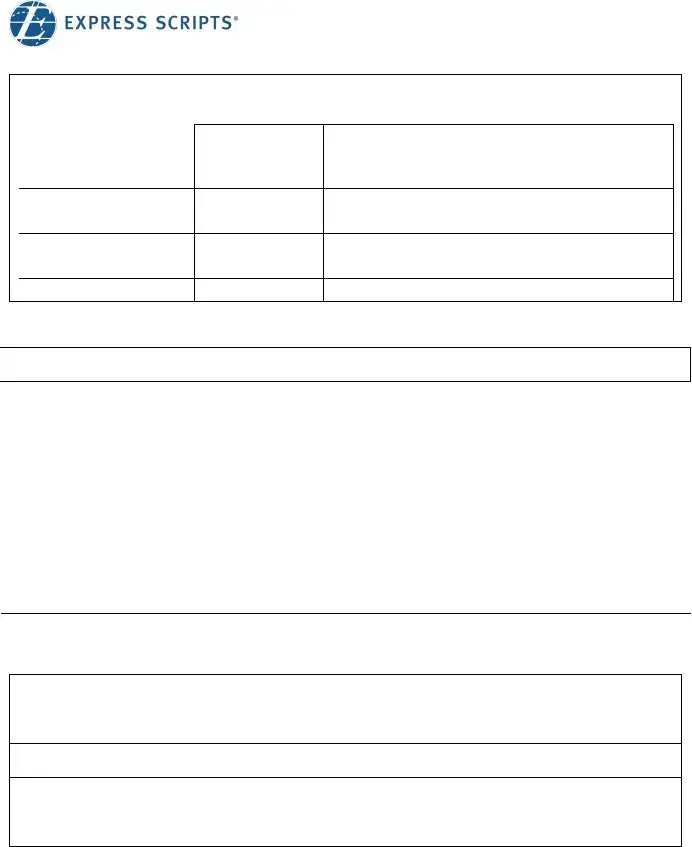
The process involves two parties: the plan member and the prescribing doctor. The plan member is responsible for completing Part A of the form, which includes personal and insurance information. After this, the plan member must take the form to their prescribing doctor, who will complete Part B, providing necessary medical information related to the medication request.
What are the steps involved in submitting the Prior Authorization form?
There are three main steps for submitting the form. First, the plan member completes Part A of the form. Second, the prescribing doctor fills out Part B. Finally, the completed form must be faxed or mailed to Express Scripts Canada. The fax number is 1 (855) 712-6329, and the mailing address is 5770 Hurontario Street, 10th Floor, Mississauga, ON L5R 3G5.
What happens after the form is submitted?
Once the form is submitted, it does not guarantee approval of the medication request. Express Scripts Canada will review the request based on predetermined clinical criteria. The plan member will receive notification regarding the approval or denial of the request. If requested, the prescribing doctor will also be informed of the decision by fax.
Can a plan member appeal a denial decision?
Yes, if a request for prior authorization is denied, the plan member has the right to appeal the decision made by Express Scripts Canada. The appeal process allows the plan member to present additional information or clarify any aspects of the initial request that may have contributed to the denial.
What information is required from the prescribing doctor?
The prescribing doctor must provide detailed information about the patient's medical condition and drug history in Part B of the form. This includes the name of the requested drug, dosage, frequency, and the medical condition for which the drug is being prescribed. The doctor must also indicate whether the drug will be used according to its Health Canada approved indications and provide relevant clinical details to support the request.
Are there any fees associated with completing the Prior Authorization form?
Yes, any fees related to the completion of the Express Scripts Prior Authorization form are the responsibility of the plan member. It is important for members to be aware of these potential costs when initiating the prior authorization process.