What is the purpose of the CNA Shower Sheets form?
The CNA Shower Sheets form is designed to assist Certified Nursing Assistants (CNAs) in conducting a thorough visual assessment of a resident's skin during showering. It helps document any abnormalities found, ensuring that they are reported to the charge nurse and addressed appropriately.
What should be included in the visual assessment?
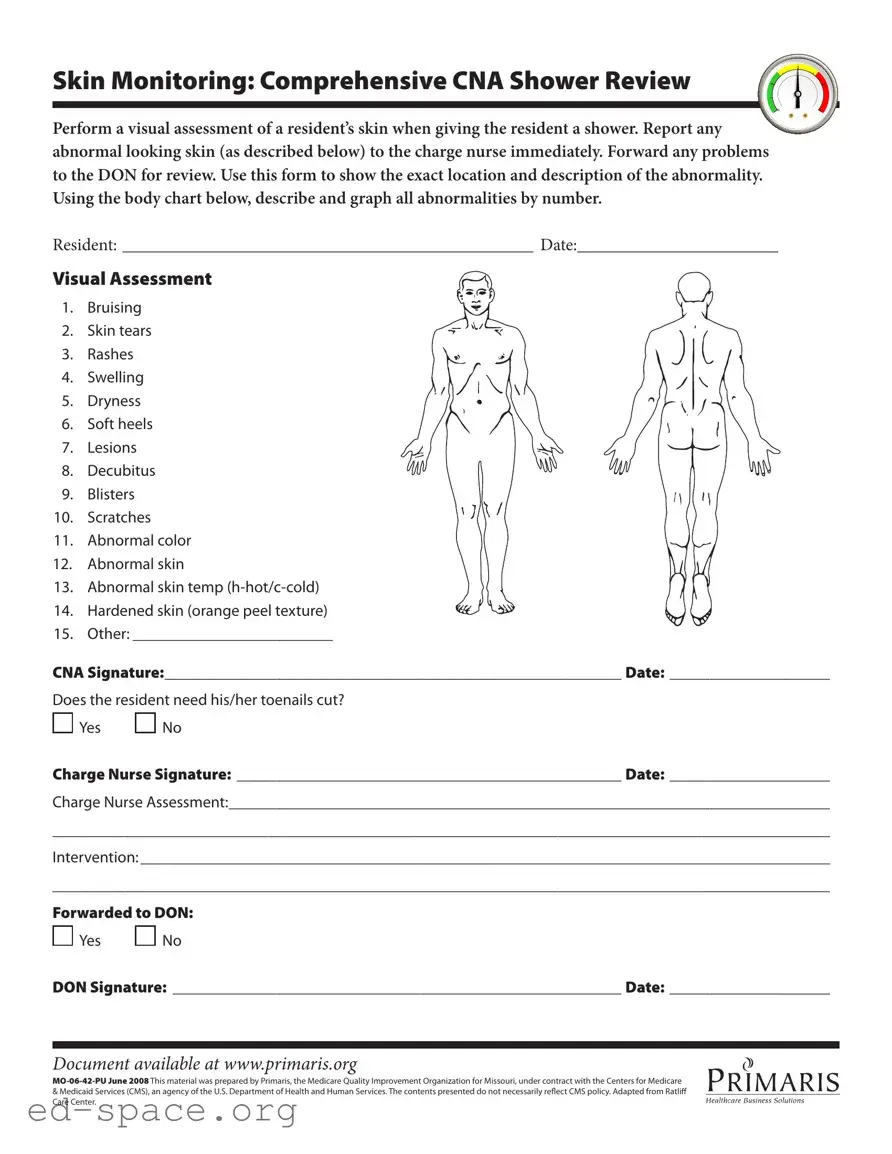
The visual assessment should include a detailed observation of the resident's skin. CNAs should look for issues such as bruising, skin tears, rashes, swelling, dryness, soft heels, lesions, decubitus ulcers, blisters, scratches, abnormal color, and abnormal temperature. Each abnormality should be documented on the form, including its exact location on the body chart provided.
How do I report abnormalities found during the assessment?
Any abnormalities observed during the skin assessment must be reported immediately to the charge nurse. It is important to provide a clear description of the issues identified. The charge nurse will then evaluate the situation and determine the next steps for intervention.
What should I do if I find an abnormality?
If an abnormality is found, the CNA should document it on the form, including its location and description. Afterward, the information should be forwarded to the Director of Nursing (DON) for further review and action.
Is there a section for documenting toenail care?
Yes, the form includes a question regarding whether the resident needs their toenails cut. CNAs should answer "Yes" or "No" based on their assessment. This information is important for the overall care of the resident.
Who signs the form after the assessment is completed?
After completing the assessment, both the CNA and the charge nurse must sign the form. The CNA's signature confirms the assessment was performed, while the charge nurse's signature indicates that they have reviewed the findings.
What happens if the charge nurse identifies additional concerns?
The charge nurse may document any additional assessments or concerns directly on the form. They will also decide on the appropriate interventions and may forward the information to the DON if necessary.
Can the form be used for multiple residents?
No, the CNA Shower Sheets form is intended for individual residents. Each form should be filled out separately to ensure accurate documentation and tracking of each resident's skin health.
Where can I find more information about the form?
Additional information about the CNA Shower Sheets form can be found at www.primaris.org. This website provides resources related to quality improvement in healthcare settings.
Is there a specific date format to use on the form?
Yes, the form requires dates to be filled out in a specific format. Ensure that the date is clearly written next to each signature and in the designated areas to maintain proper documentation.