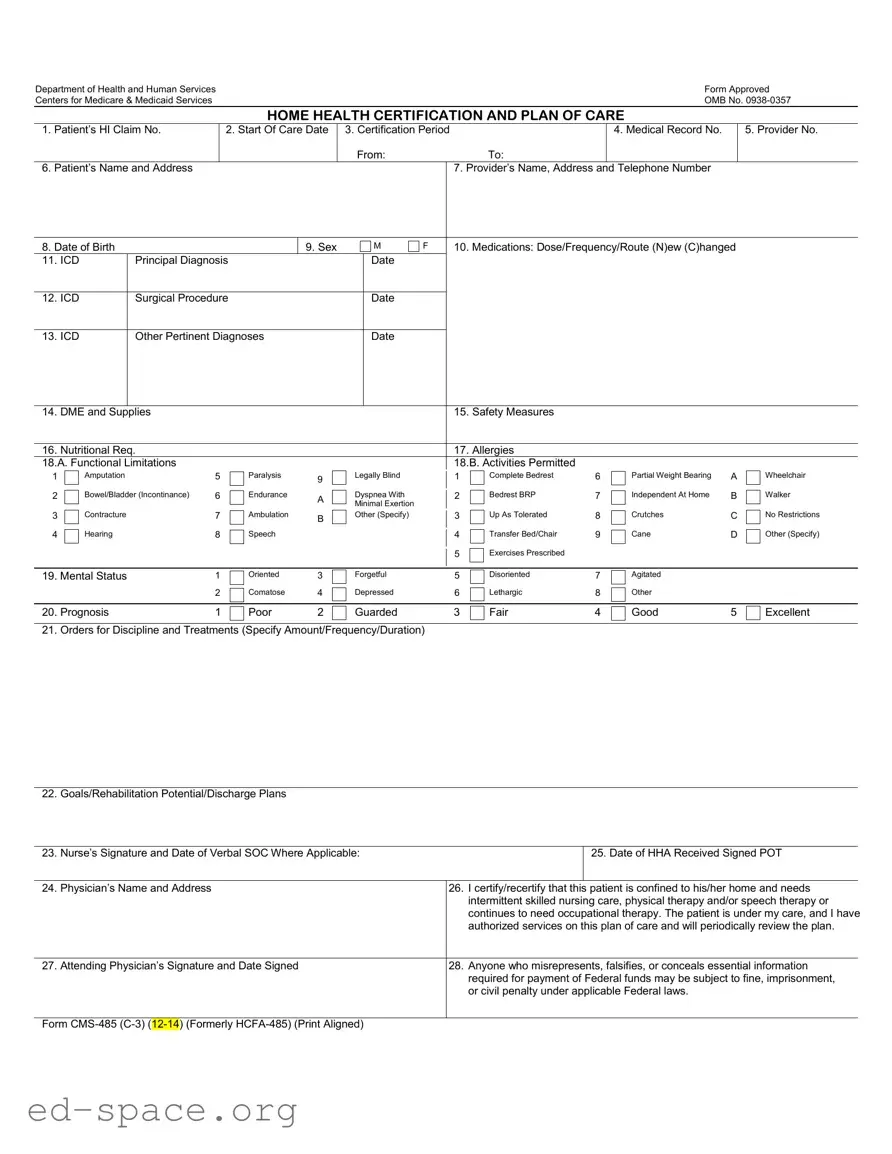
What is the CMS 485 form used for?
The CMS 485 form, also known as the Home Health Certification and Plan of Care, is utilized to certify a patient's need for home health services. It outlines the patient's medical condition, treatment plan, and the skilled services required, such as nursing care or therapy. This form is essential for Medicare reimbursement and ensures that care is delivered according to the patient's specific needs.
Who needs to sign the CMS 485 form?
The form must be signed by the attending physician who certifies that the patient is homebound and requires intermittent skilled care. The physician’s signature confirms that they have authorized the services outlined in the plan of care and will review the patient's progress periodically.
What information is required on the CMS 485 form?
The CMS 485 form requires several key pieces of information, including the patient's identification details, diagnosis codes, medications, functional limitations, and a detailed plan for care. It also includes sections for safety measures, nutritional requirements, and any allergies the patient may have. This comprehensive information helps ensure appropriate care is provided.
How often should the CMS 485 form be updated?
The CMS 485 form should be updated whenever there is a significant change in the patient's condition or care needs. Additionally, it is typically reviewed and re-signed by the physician every 60 days or as required by Medicare guidelines. Regular updates help maintain accurate and effective care plans.
What happens if the CMS 485 form is not completed correctly?
If the CMS 485 form is not completed accurately, it may lead to delays in service authorization and payment. Incomplete or incorrect information can result in denials of Medicare claims, requiring resubmission of the form. Ensuring all sections are filled out correctly is crucial for timely processing.
Is the information on the CMS 485 form confidential?
Yes, the information provided on the CMS 485 form is protected under privacy laws. The form includes a Privacy Act Statement, which outlines how the information will be used and who may have access to it. This ensures that patient information is handled with confidentiality and care.
How long does it take to complete the CMS 485 form?
Completing the CMS 485 form typically takes about 15 minutes. This estimate includes the time needed to gather necessary information, review instructions, and complete the form. It is important to allocate sufficient time to ensure accuracy and completeness.