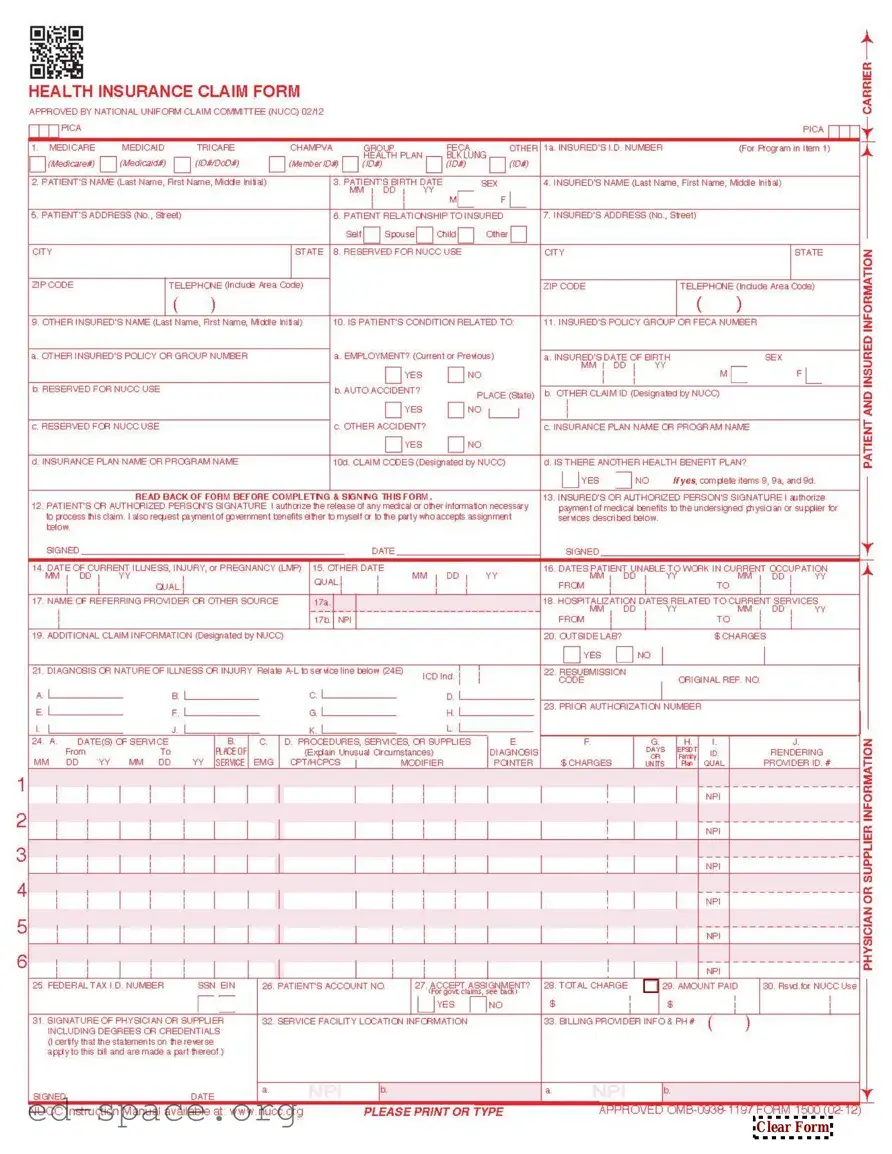
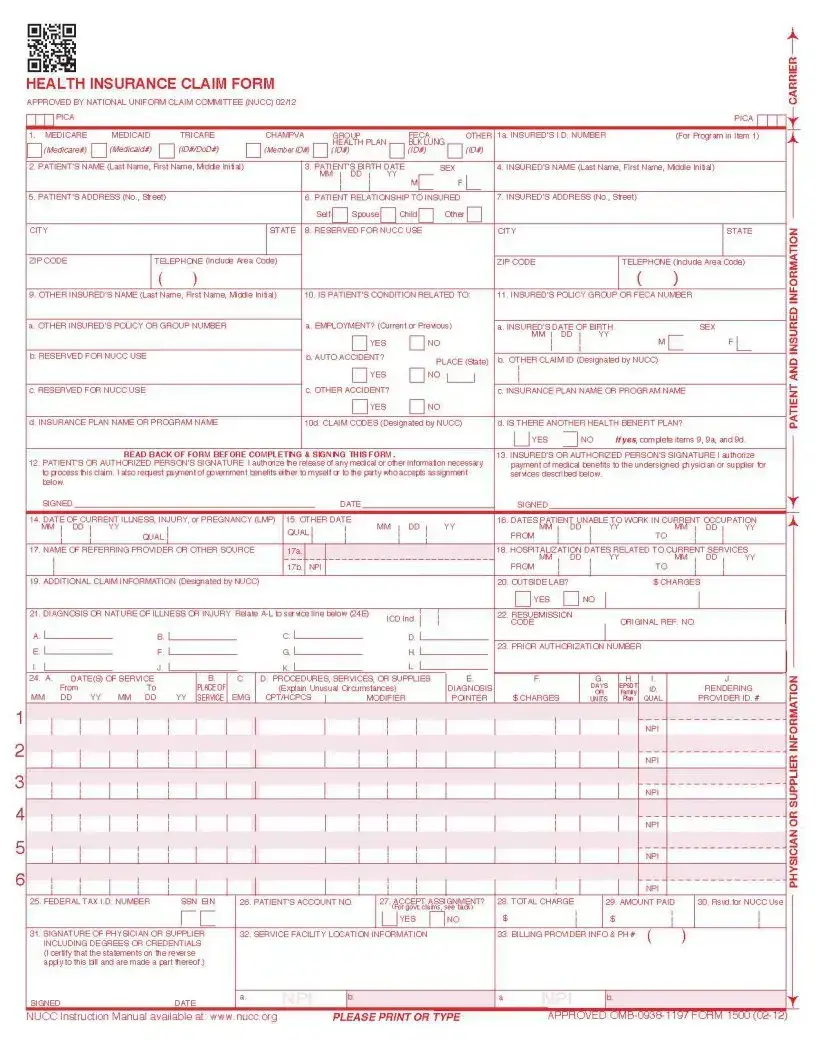
What is the CMS 1500 form?
The CMS 1500 form is a standard claim form used by healthcare providers to bill Medicare and other health insurance programs. It captures essential information about the patient, the provider, and the services rendered. This form is crucial for ensuring that healthcare providers receive payment for their services.
Who needs to use the CMS 1500 form?
Healthcare providers, including physicians, therapists, and other practitioners, use the CMS 1500 form when submitting claims for services provided to patients. It is primarily utilized by those who are not hospital-based but operate in private practice or outpatient settings.
What information is required on the CMS 1500 form?
Several key details must be included on the CMS 1500 form. This includes the patient's personal information, insurance details, the provider's information, and a description of the services provided. Specific codes for diagnoses and procedures are also necessary to process the claim accurately.
How do I fill out the CMS 1500 form correctly?
To fill out the CMS 1500 form correctly, start by gathering all necessary patient and service information. Each section of the form must be completed accurately. Use the appropriate codes for diagnoses and procedures, and ensure that the billing details match the patient’s insurance information. Double-check for any errors before submission to avoid delays in payment.
Where can I submit the CMS 1500 form?
The CMS 1500 form can be submitted electronically or via mail, depending on the insurance provider's requirements. Many providers prefer electronic submissions for faster processing. Check with the specific insurance company for their preferred submission method and guidelines.
What should I do if my claim is denied?
If a claim submitted using the CMS 1500 form is denied, review the denial notice carefully to understand the reason. Common issues include incorrect coding, missing information, or services not covered by the insurance plan. Once identified, correct the errors and resubmit the claim or appeal the denial if appropriate.