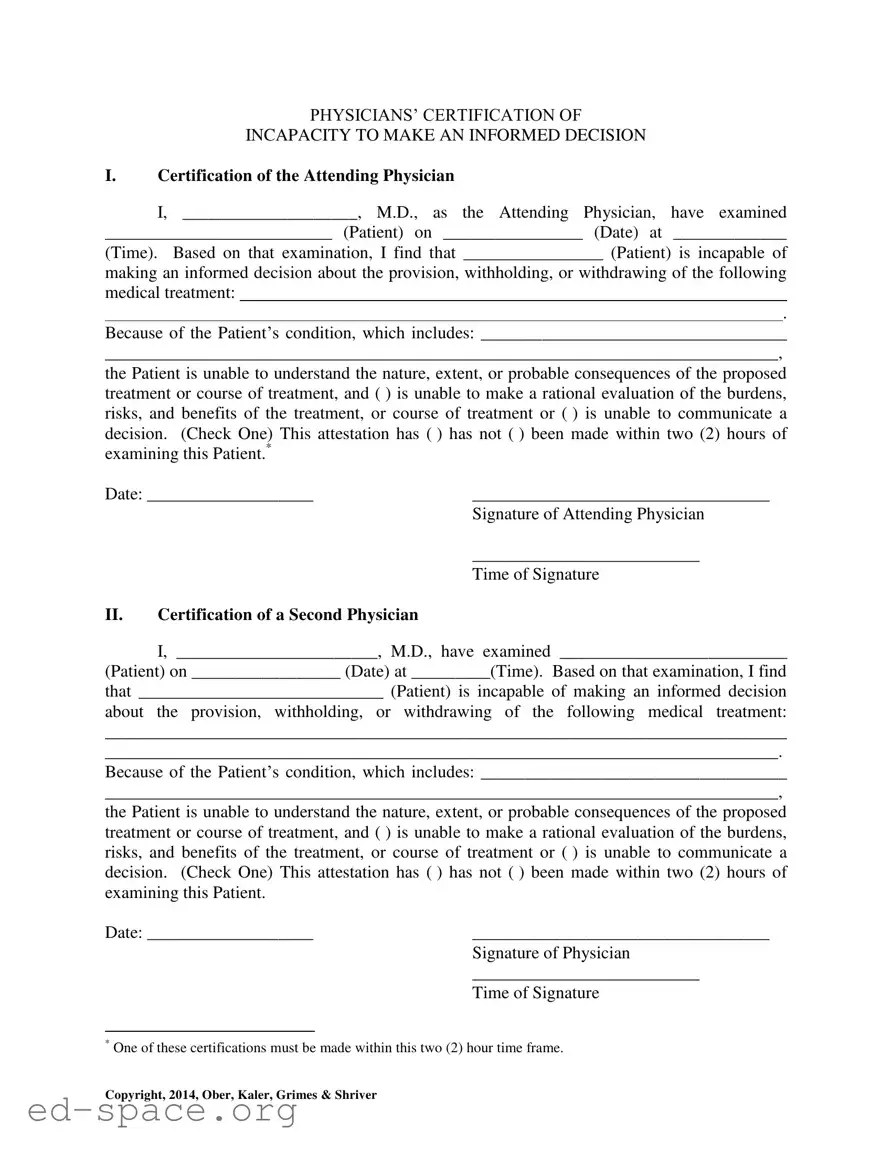
PHYSICIANS’ CERTIFICATION OF
INCAPACITY TO MAKE AN INFORMED DECISION
I.Certification of the Attending Physician
I, ____________________, M.D., as the Attending Physician, have examined
__________________________ (Patient) on ________________ (Date) at _____________
(Time). Based on that examination, I find that ________________ (Patient) is incapable of
making an informed decision about the provision, withholding, or withdrawing of the following medical treatment:
.
Because of the Patient’s condition, which includes: ___________________________________
_____________________________________________________________________________,
the Patient is unable to understand the nature, extent, or probable consequences of the proposed treatment or course of treatment, and ( ) is unable to make a rational evaluation of the burdens, risks, and benefits of the treatment, or course of treatment or ( ) is unable to communicate a decision. (Check One) This attestation has ( ) has not ( ) been made within two (2) hours of examining this Patient.*
Date: ___________________ |
__________________________________ |
|
Signature of Attending Physician |
|
__________________________ |
|
Time of Signature |
II.Certification of a Second Physician
I, _______________________, M.D., have examined __________________________
(Patient) on _________________ (Date) at _________(Time). Based on that examination, I find
that ____________________________ (Patient) is incapable of making an informed decision
about the provision, withholding, or withdrawing of the following medical treatment:
______________________________________________________________________________
_____________________________________________________________________________.
Because of the Patient’s condition, which includes: ___________________________________
_____________________________________________________________________________,
the Patient is unable to understand the nature, extent, or probable consequences of the proposed treatment or course of treatment, and ( ) is unable to make a rational evaluation of the burdens, risks, and benefits of the treatment, or course of treatment or ( ) is unable to communicate a decision. (Check One) This attestation has ( ) has not ( ) been made within two (2) hours of examining this Patient.
Date: ___________________ |
__________________________________ |
|
Signature of Physician |
|
__________________________ |
|
Time of Signature |
*One of these certifications must be made within this two (2) hour time frame.
Copyright, 2014, Ober, Kaler, Grimes & Shriver