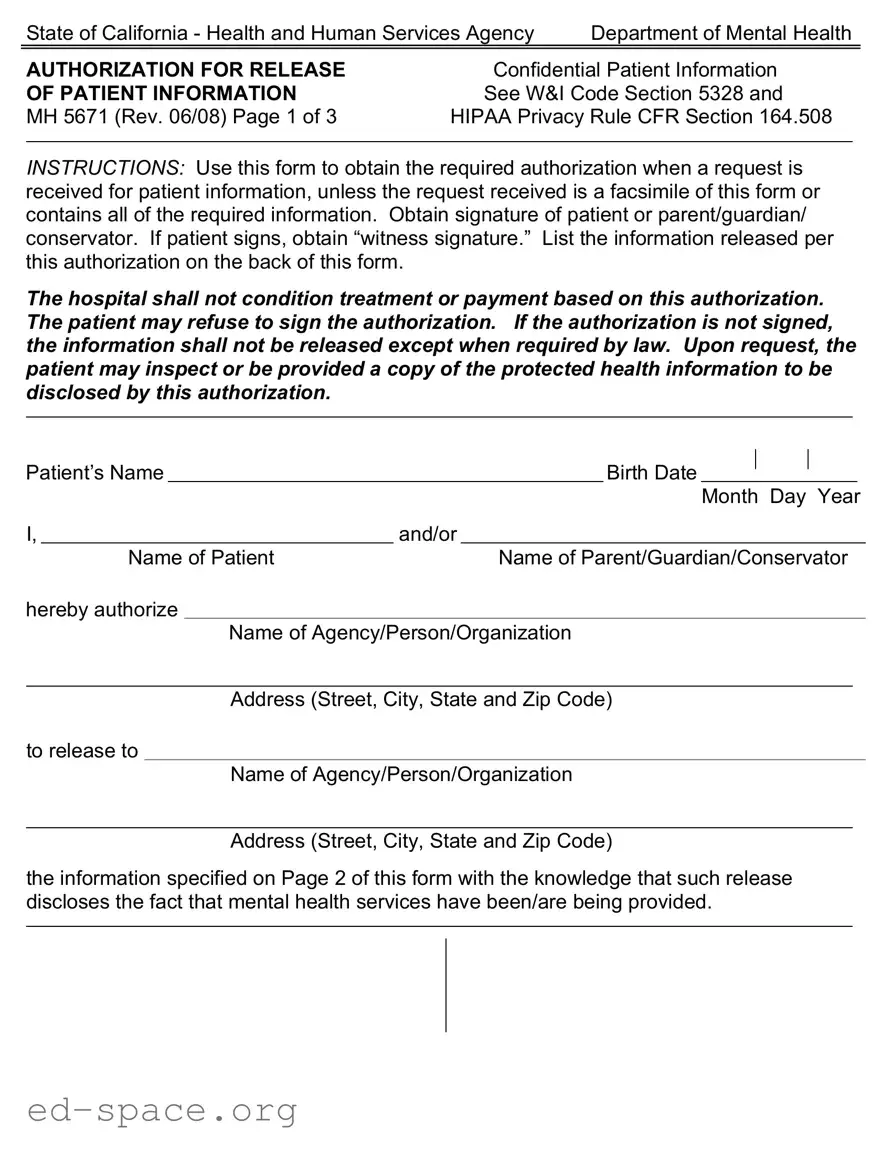
What is the purpose of the California MH 5671 form?
The California MH 5671 form is used to authorize the release of confidential patient information related to mental health services. This form ensures that patient information can be shared with specific agencies or individuals while complying with legal requirements. It is essential for protecting the privacy of the patient and ensuring that their information is only disclosed with their consent.
Who needs to sign the MH 5671 form?
The form must be signed by the patient or their parent, guardian, or conservator. If the patient is signing, a witness signature is also required. This process ensures that the patient or their representative fully understands and agrees to the release of their mental health information.
Can a patient refuse to sign the authorization?
Yes, a patient has the right to refuse to sign the authorization. If the authorization is not signed, the information will not be released unless required by law. It is important for patients to know they can exercise this right without any consequences regarding their treatment or payment.
What types of information can be released using this form?
The form allows for the release of various types of mental health information, including entire records, diagnoses, psychiatric evaluations, discharge summaries, social histories, and treatment plans. Patients can specify exactly what information they want to be disclosed by initialing the relevant sections on the form.
How long is the authorization valid?
The authorization remains effective for a specified period, which can be six months, one year, or until a date specified by the patient. If the authorization is not revoked, it will automatically terminate at the end of the chosen time frame. Patients should be aware of this duration when signing the form.
Can the patient inspect or receive a copy of their information?
Yes, patients have the right to inspect or obtain a copy of the protected health information that will be disclosed under this authorization. This provision allows patients to stay informed about their mental health records and how their information is being used.
What should be done if the patient wants to revoke the authorization?
If a patient wishes to revoke the authorization, they must do so in writing. The revocation can be made at any time, except for actions that have already been taken based on the signed authorization. It is advisable for patients to communicate their decision clearly to ensure their wishes are respected.