What is the purpose of the California Death Report form?
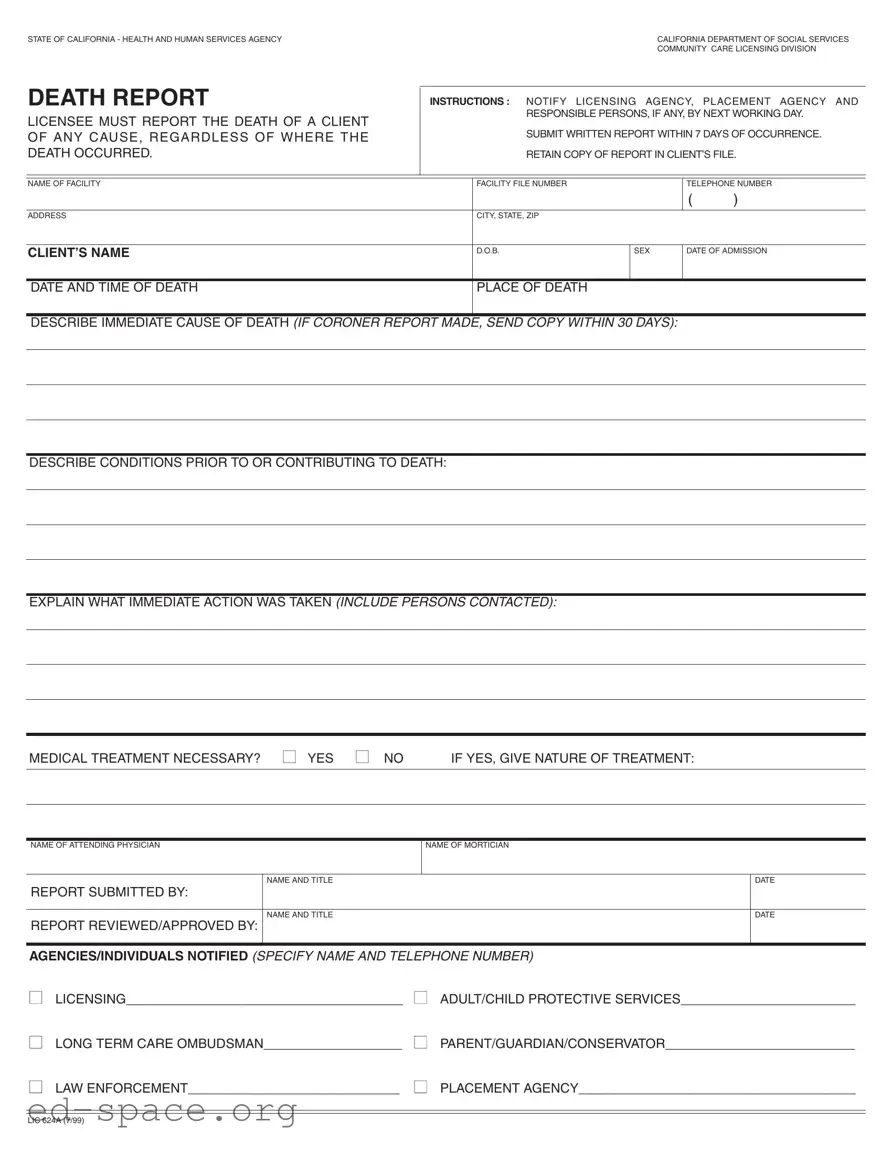
The California Death Report form is used to notify the appropriate authorities about the death of a client in a care facility. It ensures that the licensing agency, placement agency, and other responsible parties are informed promptly. The form must be submitted within seven days of the occurrence of the death, regardless of the cause or location of the event.
Who is responsible for submitting the California Death Report?
The licensee of the facility is responsible for submitting the California Death Report. Additionally, any responsible persons, if applicable, must ensure that the report is filed by the next working day following the death. This requirement emphasizes the importance of timely communication regarding client deaths.
What information is required on the form?
The form requires detailed information, including the name of the facility, facility file number, client’s name, date of birth, sex, date of admission, date and time of death, and place of death. It also asks for a description of the immediate cause of death, any contributing conditions, actions taken immediately after the death, and whether medical treatment was necessary.
What should be done if a coroner's report is available?
If a coroner's report is made, a copy must be submitted along with the California Death Report within 30 days of the occurrence. This ensures that all relevant information regarding the cause of death is available for review by the licensing agency and other involved parties.
How should the report be submitted?
What happens if the report is not submitted on time?
Failure to submit the California Death Report within the specified time frames may result in penalties for the facility. It is crucial to adhere to the reporting requirements to avoid potential legal issues and ensure compliance with state regulations.