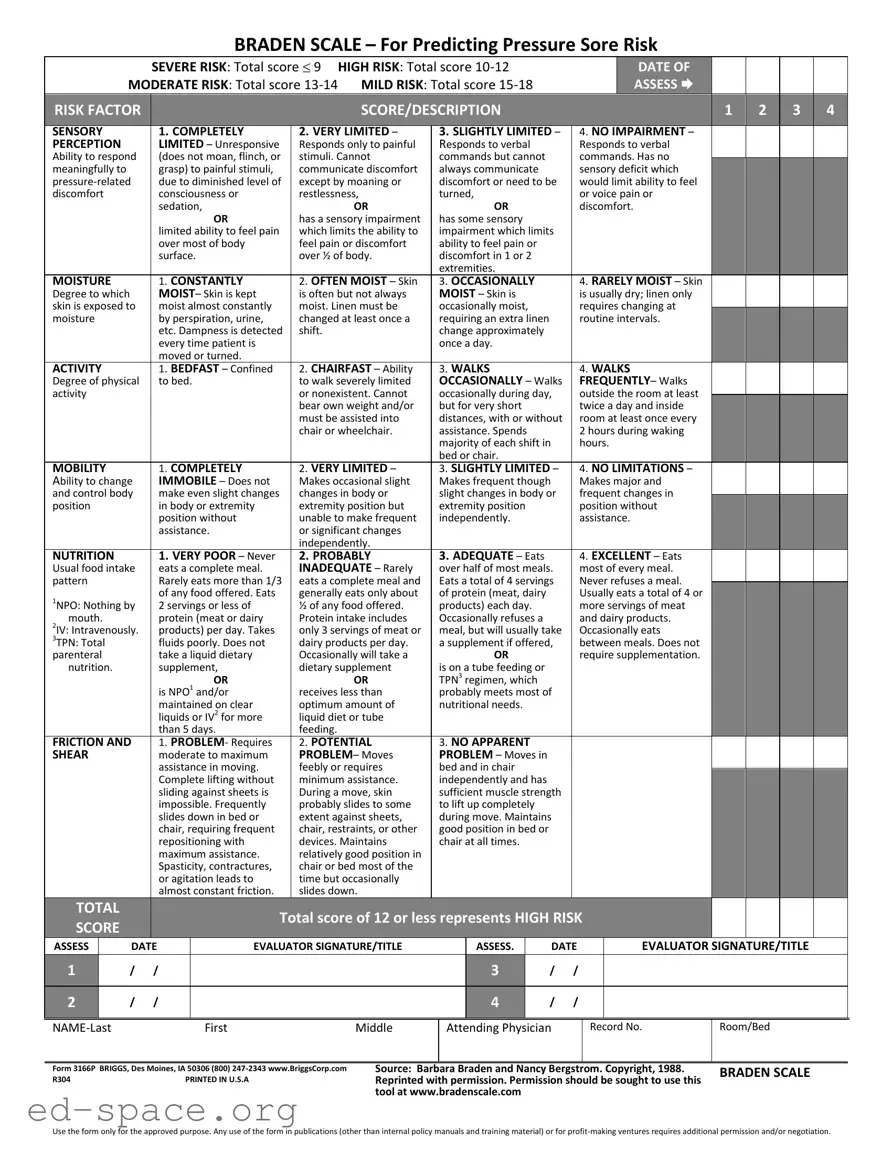
What is the Braden Scale and why is it important?
The Braden Scale is a tool used to assess a patient's risk of developing pressure sores, also known as bedsores. It evaluates six factors: sensory perception, moisture, activity, mobility, nutrition, and friction/shear. Each factor is scored, and the total score helps healthcare providers determine the level of risk. Understanding a patient's risk level is crucial for implementing preventative measures, ensuring better patient care, and reducing the occurrence of pressure sores.
How is the Braden Scale scored?
The Braden Scale uses a scoring system ranging from 6 to 23. Each of the six factors is assigned a score based on the patient's condition. Lower total scores indicate a higher risk for pressure sores. For example, a score of 9 indicates severe risk, while a score of 15-18 indicates mild risk. This scoring system allows healthcare providers to quickly assess and categorize a patient's risk level, guiding their care decisions.
Who should use the Braden Scale?
The Braden Scale is primarily used by healthcare professionals, including nurses and physicians, in various settings such as hospitals, nursing homes, and home care. It is essential for any caregiver responsible for patients who may be at risk for pressure sores, particularly those with limited mobility, poor nutrition, or sensory impairments. Training on how to use the scale effectively is recommended for accurate assessments.
How often should the Braden Scale be assessed?
Assessment frequency depends on the patient's condition and risk factors. Generally, it is recommended to assess patients at least once per shift or whenever there is a change in their condition. Regular assessments allow healthcare providers to monitor changes in risk levels and adjust care plans accordingly, ensuring timely interventions to prevent pressure sores.
What should be done if a patient is assessed as high risk?
If a patient is identified as high risk on the Braden Scale, immediate action is necessary. Care plans should include interventions such as regular repositioning, use of pressure-relieving devices, and nutritional support. Education for both staff and family members about the importance of prevention strategies is also crucial. By proactively addressing the identified risks, healthcare providers can significantly reduce the likelihood of pressure sore development.