What is a Do Not Resuscitate (DNR) Order in Arkansas?
A Do Not Resuscitate Order is a legal document that allows individuals to refuse cardiopulmonary resuscitation (CPR) and other life-saving measures in the event of cardiac arrest or respiratory failure. In Arkansas, this order must be completed by a physician and signed by the patient or their legal representative.
Who can request a DNR Order?
Any adult who is capable of making their own medical decisions can request a DNR Order. Additionally, a legal representative, such as a healthcare proxy or power of attorney, may also request this order on behalf of an individual who is unable to make decisions.
How is a DNR Order created in Arkansas?
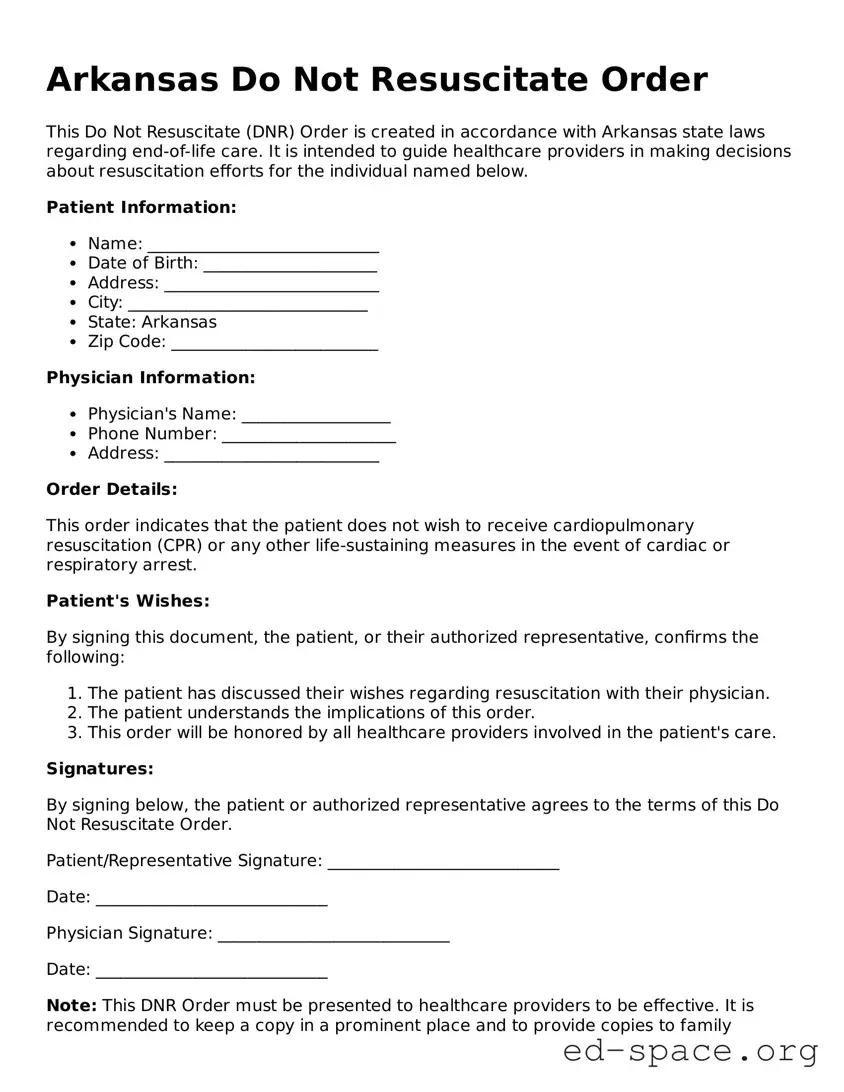
To create a DNR Order, the patient must discuss their wishes with a physician. The physician will then complete the official DNR form, which must be signed by both the physician and the patient or their legal representative. It is important that the form is filled out correctly to ensure its validity.
Where should the DNR Order be kept?
The DNR Order should be kept in a location that is easily accessible to medical personnel, such as on the refrigerator, in a medical file, or with the individual at all times. It is advisable to inform family members and caregivers about the location of the document.
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time by the patient or their legal representative. To revoke the order, the individual should inform their healthcare provider and remove or destroy the DNR form. It is important to ensure that all relevant parties are informed of the revocation.
Does a DNR Order apply outside of a hospital setting?
In Arkansas, a DNR Order is generally applicable in both hospital and out-of-hospital settings. However, it is important to confirm that emergency medical services (EMS) are aware of the DNR Order and understand its terms, especially in non-hospital environments.
What happens if a DNR Order is not honored?
If a DNR Order is not honored, it may lead to unnecessary resuscitation efforts, which can cause distress to the patient and their family. In such cases, legal action may be considered, as failing to comply with a valid DNR Order can be viewed as a violation of the patient's rights.
Are there any specific requirements for the DNR form in Arkansas?
The DNR form in Arkansas must include the patient's name, the physician's name, and the signatures of both parties. It should also clearly state the patient's wishes regarding resuscitation. The form must comply with state regulations to be considered valid.
Can family members override a DNR Order?
Family members cannot override a DNR Order that has been properly executed by the patient and their physician. However, if the patient is unable to communicate, family members may be consulted about the patient's wishes, but the legally binding DNR remains in effect.
How can I obtain a DNR Order form in Arkansas?
A DNR Order form can be obtained from healthcare providers, hospitals, or the Arkansas Department of Health. It is advisable to consult with a physician to ensure that the form is completed correctly and reflects the individual's wishes accurately.