What is a Do Not Resuscitate Order (DNR) in Arizona?
A Do Not Resuscitate Order (DNR) in Arizona is a legal document that allows a person to refuse resuscitation efforts in the event of a medical emergency. This means that if a person’s heart stops beating or they stop breathing, medical personnel will not perform cardiopulmonary resuscitation (CPR) or other life-saving measures. The order is typically used by individuals with terminal illnesses or those who wish to avoid aggressive medical interventions at the end of life.
How do I obtain a DNR form in Arizona?
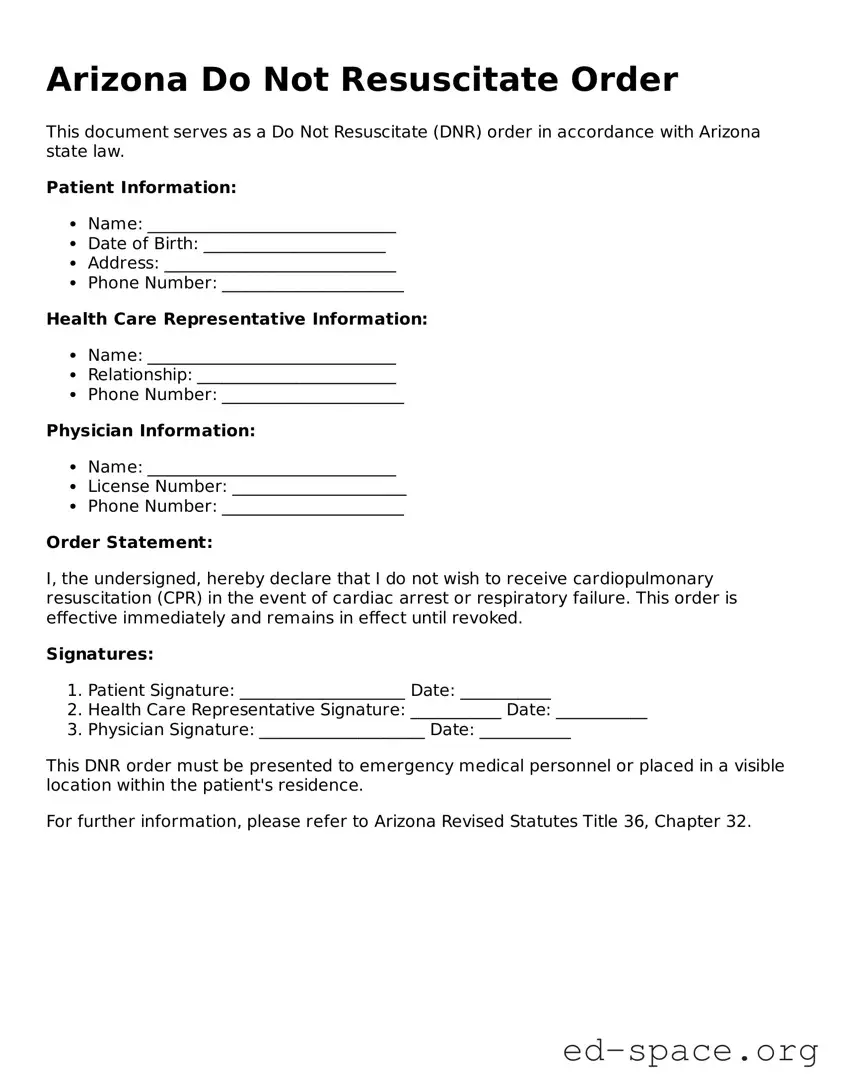
To obtain a DNR form in Arizona, individuals can download it from the Arizona Department of Health Services website or request a copy from their healthcare provider. It is important to ensure that the form is the most current version. Once completed, the form must be signed by the patient and a physician to be valid.
Who can sign a DNR order?
A DNR order can be signed by the patient themselves if they are of sound mind and able to make their own medical decisions. If the patient is unable to sign, a legally authorized representative, such as a healthcare proxy or family member, may sign on their behalf. It is essential that the person signing the order understands the implications of the decision.
Is a DNR order valid in all healthcare settings?
Yes, a DNR order is valid in all healthcare settings in Arizona, including hospitals, nursing homes, and at home. However, it is crucial to ensure that the order is clearly visible and accessible to medical personnel. Carrying a copy of the DNR order or wearing a medical alert bracelet can help ensure that healthcare providers are aware of the patient’s wishes.
Can a DNR order be revoked?
Yes, a DNR order can be revoked at any time by the patient or their authorized representative. To revoke the order, the individual should destroy the original document and inform their healthcare provider of the change. It is advisable to create a new order if the patient’s wishes change regarding resuscitation.
What should I discuss with my doctor before completing a DNR order?
Before completing a DNR order, it is important to have an open discussion with your doctor about your medical condition, prognosis, and treatment options. Understanding the implications of a DNR order and how it aligns with your personal values and wishes is essential. Your doctor can help clarify any questions and provide guidance on end-of-life care decisions.
Are there any other documents related to end-of-life decisions I should consider?
Yes, in addition to a DNR order, individuals may want to consider creating an advance directive or a living will. These documents outline your preferences for medical treatment and appoint someone to make healthcare decisions on your behalf if you become unable to do so. It is advisable to discuss these documents with your healthcare provider to ensure they align with your wishes.