What information is needed to fill out the Annual Physical Examination form?
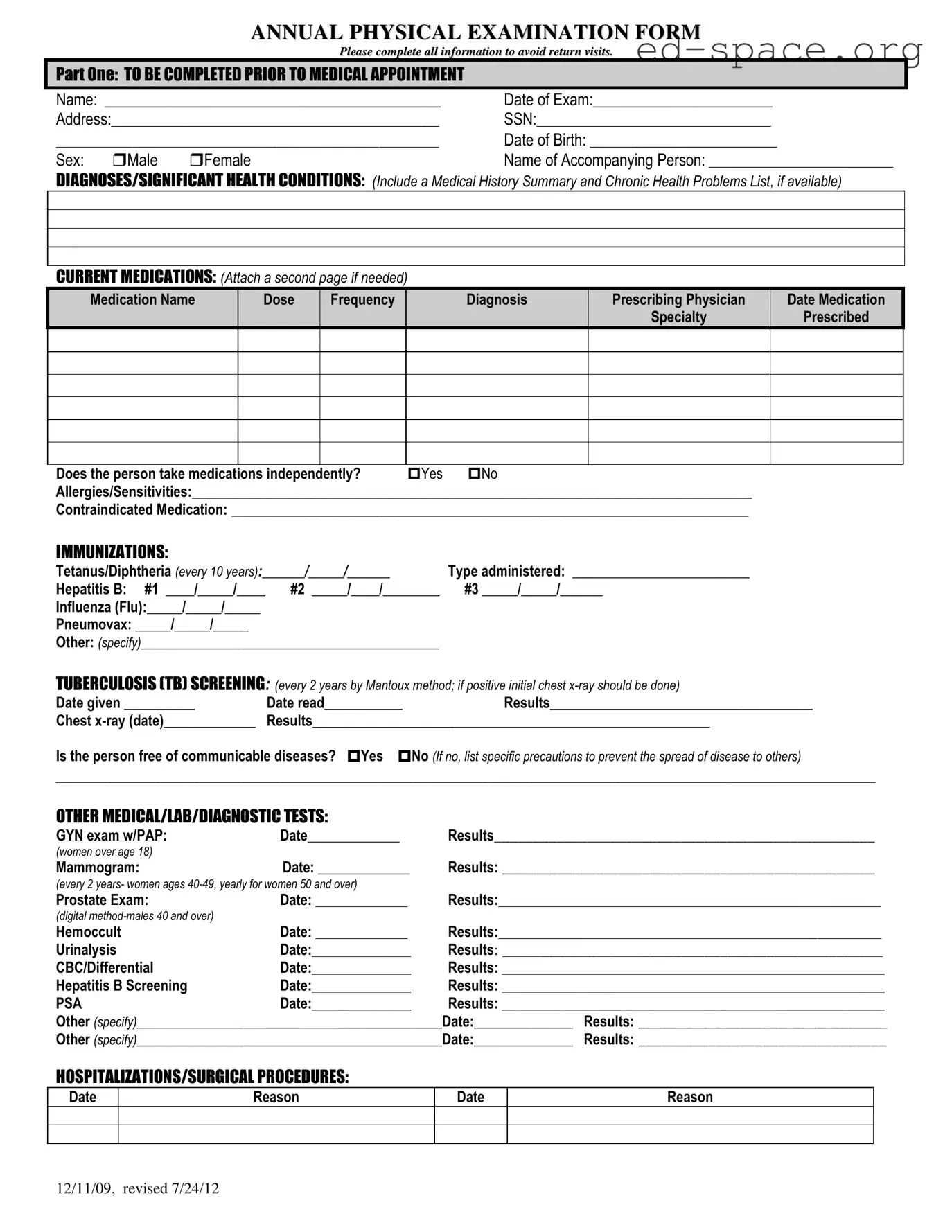
To complete the Annual Physical Examination form correctly, it requires an array of detailed information. Firstly, personal identification details such as name, date of the exam, address, Social Security Number (SSN), date of birth, and sex need to be filled out. You should also provide the name of any accompanying person. The health-related sections call for a comprehensive medical history including diagnoses/significant health conditions, a list of current medications specifying each medication's name, dose, frequency, prescribing physician, and the date it was prescribed. It also requires information on whether medications are taken independently, any allergies or medications that are contraindicated, immunization records, TB screening results, and results of other medical, lab, or diagnostic tests. The form further asks about hospitalizations/surgical procedures, general physical exam results including blood pressure and temperature, an evaluation of various body systems, and details regarding vision and hearing screening. Finally, it solicits information on health maintenance recommendations, any limitations or restrictions for activities, the use of any adaptive equipment, changes in health status, and recommendations for specialty consults.
How often should TB screening be done according to the form?
According to the Annual Physical Examination form, TB (Tuberculosis) screening should be conducted every 2 years. This screening is recommended to be performed using the Mantoux method. If the initial screening results are positive, a chest x-ray should be done to further assess the individual's health status regarding TB.
Are there specific guidelines for women's health screening mentioned in the form?
Yes, the form outlines specific health screening guidelines for women. It mentions that women over the age of 18 should have a GYN exam with a PAP smear. Meanwhile, mammograms are recommended every 2 years for women aged 40-49 and yearly for women aged 50 and over. These screenings are important parts of preventative health measures for women, helping to detect potential issues early.
What should you do if you need more space for the medication section?
If you find that the current medications section on the form does not provide enough space for your needs, you are encouraged to attach a second page to list all medications adequately. This ensures that your health care provider has a comprehensive understanding of your current medications, including the names, dosages, frequencies, diagnoses, prescribing physicians, and dates prescribed. Providing complete information is crucial for accurate medical review and care.