What is the Alabama 369 form used for?
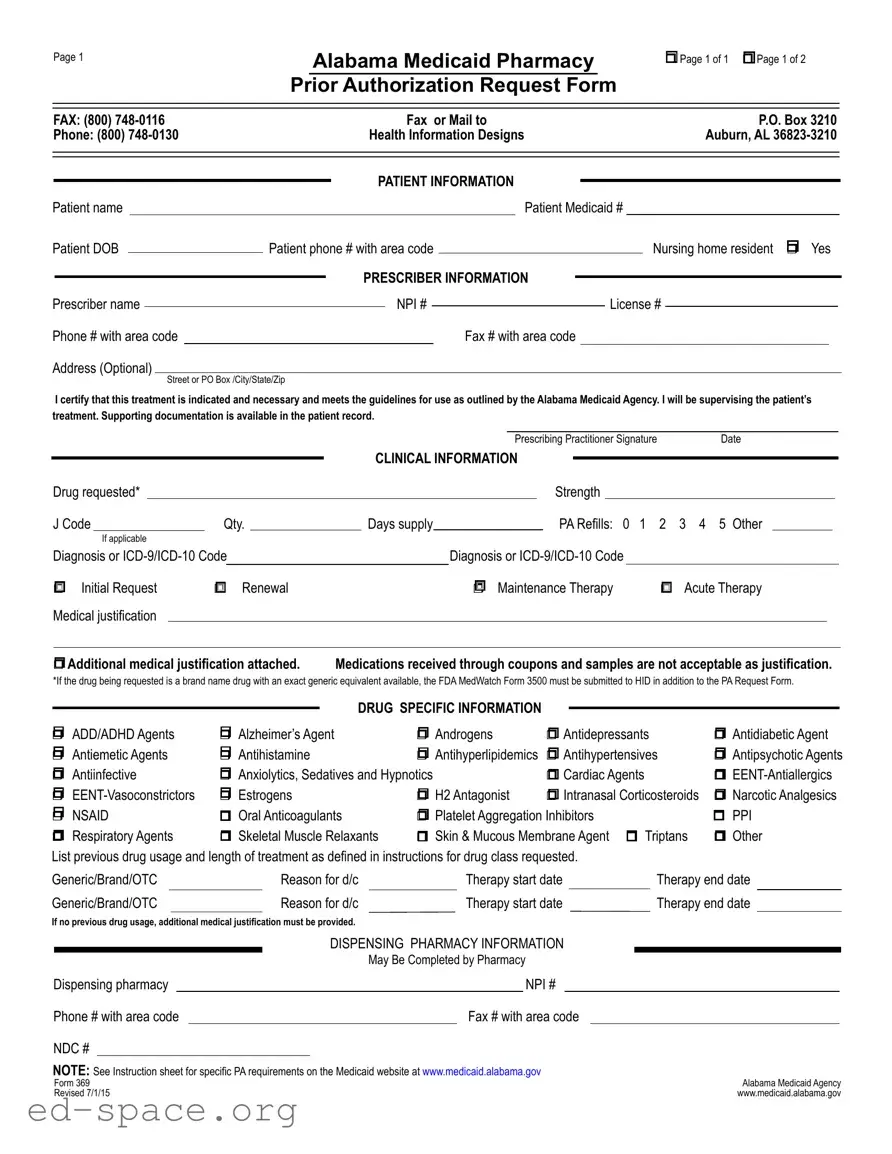
The Alabama 369 form is primarily utilized for requesting prior authorization for pharmacy services under the Alabama Medicaid program. This form is essential for healthcare providers to obtain approval for specific medications that may not be automatically covered by Medicaid. By submitting this form, prescribers can demonstrate that a particular treatment is medically necessary and adheres to the guidelines set forth by the Alabama Medicaid Agency.
Who needs to fill out the Alabama 369 form?
The form must be completed by the prescriber, who is responsible for the patient's treatment. This includes physicians, nurse practitioners, and physician assistants. It requires detailed patient information, including the patient's Medicaid number, date of birth, and contact details. Additionally, the prescriber must provide their own information, including their name, National Provider Identifier (NPI), and license number.
What information is required on the Alabama 369 form?
Several key pieces of information are needed on the Alabama 369 form. This includes the patient's demographics, the medication requested, its strength, quantity, and the diagnosis codes. The prescriber must also indicate whether the request is for an initial request, renewal, or maintenance therapy. Medical justification for the requested medication must be provided, along with any previous drug usage history if applicable. Supporting documentation may also be required to substantiate the request.
How is the Alabama 369 form submitted?
The completed Alabama 369 form can be submitted via fax or mail. The fax number for submissions is (800) 748-0116, and it can also be mailed to Health Information Designs at P.O. Box 3210, Auburn, AL 36823-3210. It’s crucial to ensure that all required information is accurately filled out to avoid delays in processing the authorization request.
What happens after the Alabama 369 form is submitted?
Once the form is submitted, the Alabama Medicaid Agency will review the request to determine if the medication meets the necessary criteria for coverage. The prescriber will receive notification regarding the approval or denial of the request. If approved, the patient can proceed to obtain the medication. If denied, the prescriber may need to provide additional information or consider alternative treatments.