Member’s Name (For faxing purpose):
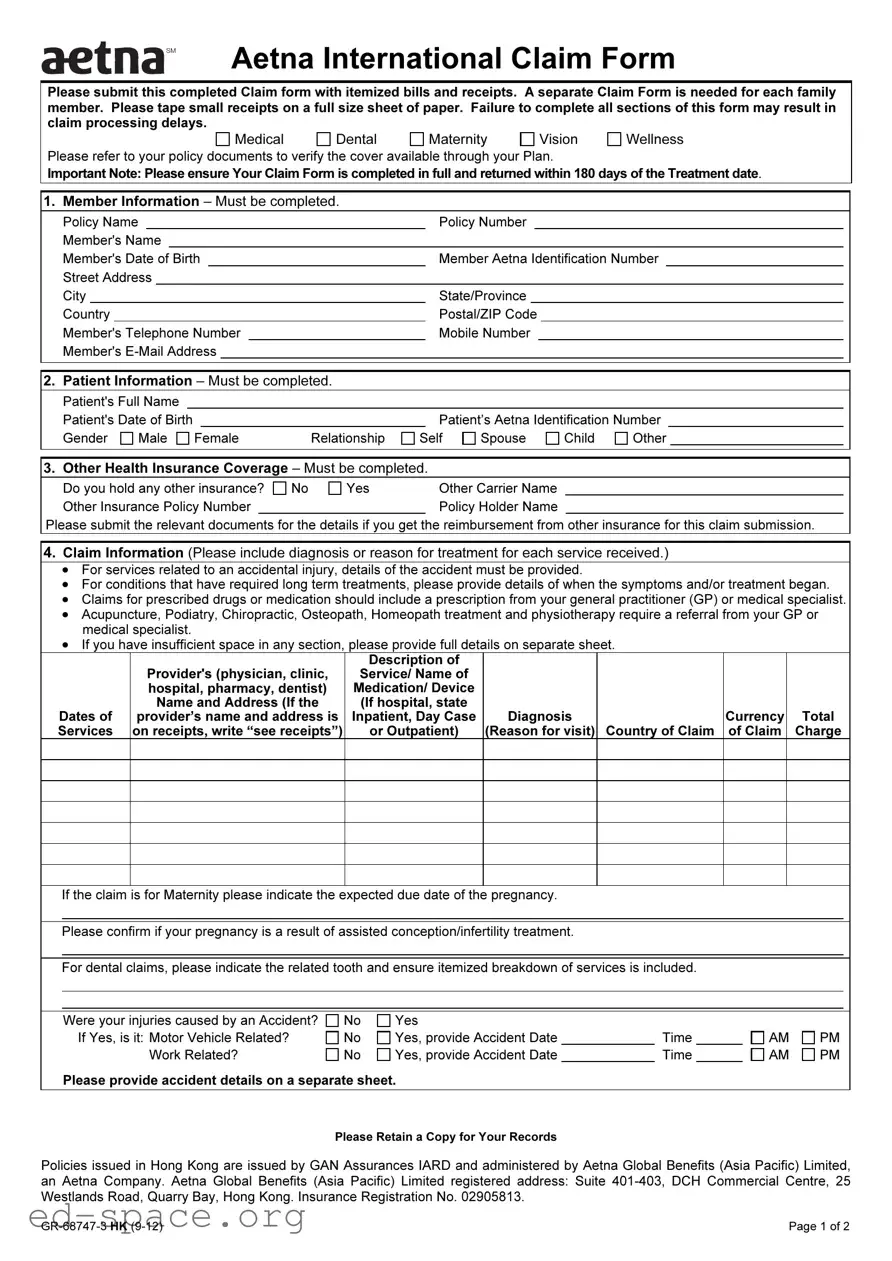
5. Summary of Payment Details – Must be completed.
Recurring Reimbursement Election – Please check one of the following options if you want to:
Receive future payments using the details provided below
Use the payment information provided below for this claim only
Use the payment details that we already have on file for you
Payment Information
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Please select your preferred reimbursement method: |
Bank Transfer |
Cheque |
|
|
|
|
|
(If no selection is made, the default method is cheque issued in the member’s name.) |
|
|
|
|
|
Please indicate your preferred payment currency (If none is indicated, the default currency is US Dollar.) |
|
|
|
|
Payee Name |
|
|
|
|
Specify if: |
Member |
Provider |
Employer |
|
|
Claim Settlement Address (if different to Section 1): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Street |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City |
|
|
State/Province |
Country |
|
|
|
|
If you have selected Bank Transfer as your preferred payment method, the following information is required: |
|
|
|
Bank Account Holder Name (as per Bank Statement) |
|
|
|
|
|
|
|
|
|
|
|
|
Bank Account Number |
|
|
|
Sort Code/Branch Code |
|
|
|
|
|
|
IBAN Code* |
|
|
|
Swift/BIC Code |
|
|
|
|
|
|
IFSC/ABA/ US Routing Code |
|
|
|
|
|
|
|
|
|
|
|
|
Bank Name |
|
|
|
|
|
|
|
|
|
|
|
|
Bank Address (include Country)
Bank Telephone Number (include Country Code)
*The IBAN is mandatory for bank transfer claim payment transactions in certain countries, such as the United Arab Emirates (UAE). This must be supplied if you are using a bank account in one of these countries. Members should check with their bank to confirm any IBAN requirements.
The most efficient method of receiving your benefits reimbursement is via Bank Transfer. Please check with your bank for help with providing the appropriate instructions to Aetna International.
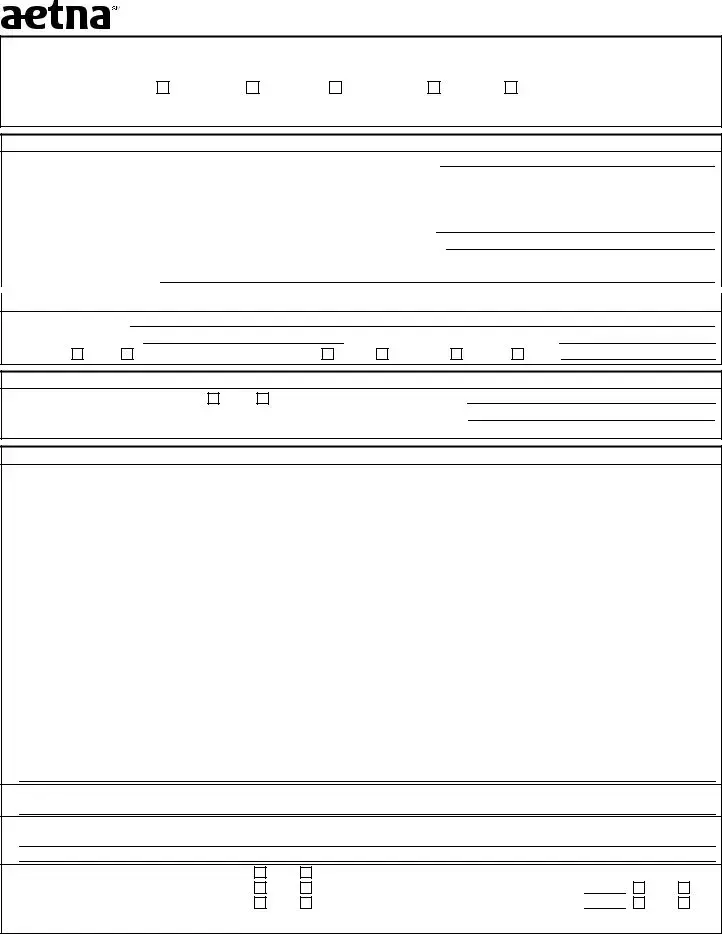
6.Declaration – Must be completed.
I declare that, to the best of my knowledge, all the information provided on this claim form is truthful and correct. I understand that Aetna will rely on the information provided as such. I agree and accept that this declaration gives Aetna, and its appointed representatives, the right to request past, present, and future medical information in relation to this claim, or any other claim related to the member/covered individual, from any third party, including providers and medical practitioners. I declare and agree
that personal information may be collected, held, disclosed, or transferred (worldwide) to any organization within the Aetna group, its suppliers, providers and any affiliates.
Patient's Signature |
|
Date |
(If patient is under 18 years of age, Parent or Guardian must sign.) |
|
Important Note: Please ensure Your Claim Form is completed in full and returned within six months (180 days) of the Treatment date. Failure to complete your form in full will result in the form being returned to you and will delay the processing of your claim. Please note Aetna International is not responsible for any costs associated with the completion of this form or for any further information/ document requested by Us to assess Your claim. The issuing of this Claim Form is in no way an admission of liability.
Please refer to your Member Handbook under General Claims Information for In-Patient, Day-Patient, Out-Patient Treatment and Pre-authorizations for all MRI and CT scans.
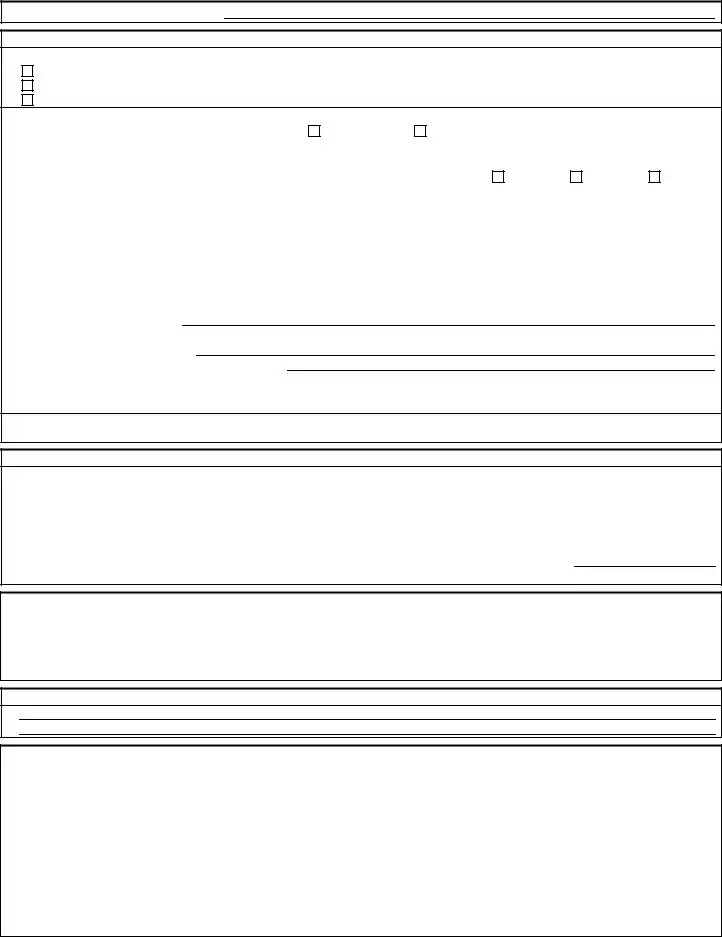
7. Additional Information
How to submit a Claim
Aetna International provides alternative methods of submitting a claim form to make it easier for our members, below are the listed options:
• Postal Submission |
• Online Claim Submission for our members via our |
Aetna Global Benefits (Asia Pacific) Limited |
secure portal |
Suite 401-403 |
www.AetnaInternational.com |
DCH Commercial Centre |
• Submit your claim via Fax attaching receipts and |
25 Westlands Road |
referrals from your Medical Practitioner |
Quarry Bay |
+852-2866-2555 |
Hong Kong |
• Email Submission with copies of your receipts and |
|
referrals from your Medical Practitioner |
|
[email protected] |
|
• For claim related queries please contact our 24 hour |
|
Member Services helpline |
|
+852-3071-5022 |
Please Retain a Copy for Your Records
Policies issued in Hong Kong are issued by GAN Assurances IARD and administered by Aetna Global Benefits (Asia Pacific) Limited, an Aetna Company. Aetna Global Benefits (Asia Pacific) Limited registered address: Suite 401-403, DCH Commercial Centre, 25 Westlands Road, Quarry Bay, Hong Kong. Insurance Registration No. 02905813.