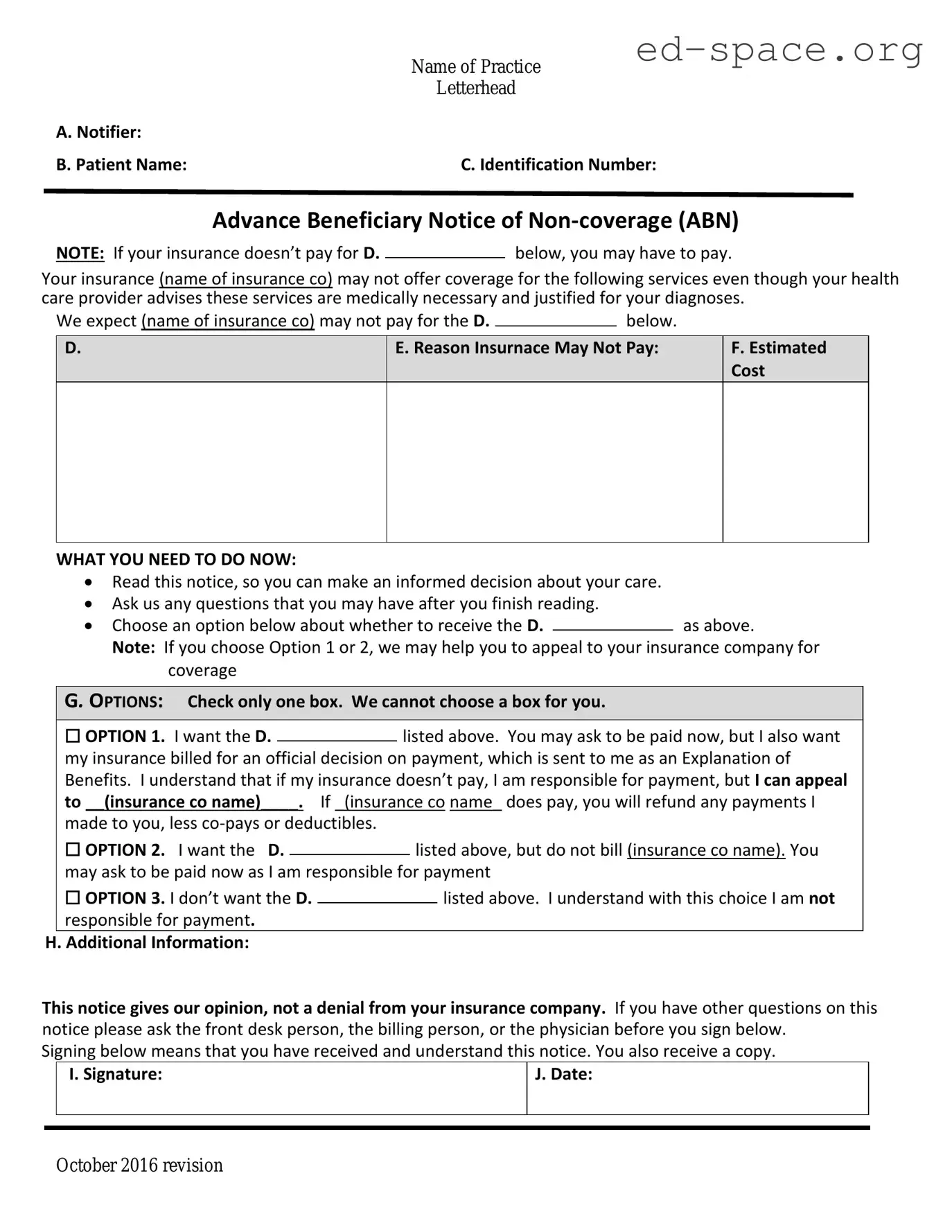
A. Notifier:
B. Patient Name: C. Identification Number:
Advance Beneficiary Notice of Non-coverage
(ABN)
NOTE: If Medicare doesn’t pay for D.____________ below, you may have to pay.
Medicare does not pay for everything, even some care that you or your health care provider have
good reason to think you need. We expect Medicare may not pay for the D. _________below.
E. Reason Medicare May Not Pay:
WHAT YOU NEED TO DO NOW:
•
Read this notice, so you can make an informed decision about your care.
•
Ask us any questions that you may have after you finish reading.
•
Choose an option below about whether to receive the D. listed above.
Note: If you choose Option 1 or 2, we may help you to use any other insurance that you
might have, but Medicare cannot require us to do this.
G. OPTIONS: Check only one box. We cannot choose a box for you.
□
OPTION 1. I want the D. listed above. You may ask to be paid now, but I
also want Medicare billed for an official decision on payment, which is sent to me on a Medicare
Summary Notice (MSN). I understand that if Medicare doesn’t pay, I am responsible for
payment, but I can appeal to Medicare by following the directions on the MSN. If Medicare
does pay, you will refund any payments I made to you, less co-pays or deductibles.
□
OPTION 2. I want the D. listed above, but do not bill Medicare. You may
ask to be paid now as I am responsible for payment. I cannot appeal if Medicare is not billed.
□
OPTION 3. I don’t want the D. listed above. I understand with this choice I
am not responsible for payment, and I cannot appeal to see if Medicare would pay.
H. Additional Information:
Thi
s notice gives our opinion, not an official Medicare decision. If you have other questions on this
notice or Medicare billing, call 1-800-MEDICARE (1-800-633-4227/TTY: 1-877-486-2048).
Signing below means that you have received and understand this notice. You may ask to receive a copy.
You have the right to get Medicare information in an accessible format, like large print, Braille, or audio. You
also have the right to file a complaint if you feel you’ve been discriminated against. Visit Medicare.gov/about-
us/accessibility-nondiscrimination-notice.
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number.
The valid OMB control number for this information collection is 0938-0566. The time required to complete this information collection is estimated to average 7 minutes
per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If
you have comments concerning the accuracy of the time estimate or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA
Reports Clearance Officer, Baltimore, Maryland 21244-1850.
Form CMS-R-131 (Exp.01/31/2026) Form Approved OMB No. 0938-0566